Chapter 5
Barriers to accessing mental health services
Introduction
5.1
This chapter considers the barriers to accessing mental health services
for ADF members and veterans, primarily their reluctance to seek help. It also
focuses on the difficulties and challenges experienced by ADF members and
veterans in seeking assistance through Department of Veterans' Affairs (DVA)
delivery models and claims processes, including ADF members and veterans who
live in regional and remote areas.
Stigma and perceived barriers to care
ADF members
5.2
As discussed in previous chapters, both Defence and DVA agree that early
identification and treatment of mental ill-health is essential for achieving
the best outcomes for ADF members and veterans with mental ill-health. However,
the 2010 ADF Mental Health Prevalence and Wellbeing Study (MHPW study) found
that 'a significant number of personnel with mental disorders had received no
care in the previous 12 months'.[1]
The MHWP study found potential stigma to be a 'substantial issue', which
limited the probability that ADF members would seek treatment for mental
ill-health,[2]
explaining that:
Research indicates that two main factors contribute to the
low uptake of mental health care: the fear of stigma and perceived barriers to
care. Stigma is a negative attitude resulting from the acceptance and
internalisation of 'prejudice or negative stereotyping', while barriers to care
are the organisational, procedural or administrative aspects of access to
mental health care that may preclude or reduce access to mental health
treatment and support. Barriers may include issues associated with
confidentiality, anonymity and confidence in the mental health service
providers. These are influenced to varying degrees by internalised stigmas
about access to care and the consequences of asking for help.[3]
5.3
The MHWP study found that among its respondents, the highest rated
barrier to personnel seeking help for a 'stress-related, emotional, mental
health or family problem' in the ADF was the concern that seeking help would
reduce their deployability (36.9 per cent). The highest perceived stigma that
concerned members was that people would treat them differently (27.6 per cent)
and that seeking care would harm their careers (26.9 per cent). The findings
are outlined in Figure 5.1.
Figure 5.1 – Estimated prevalence
of stigma and barriers to care, by rank
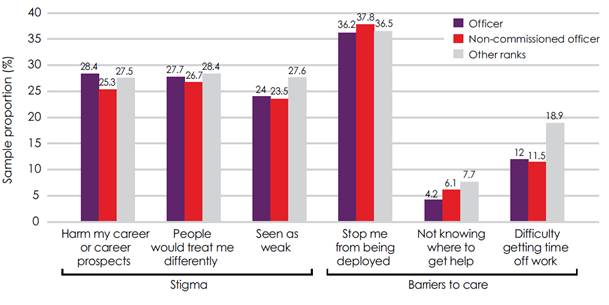
Department of Defence, Mental
Health in the Australian Defence Force: 2010 ADF Mental Health Prevalence and
Wellbeing Study Report, p. xxix.
5.4
A significant number of submissions also identified stigma surrounding
mental ill-health and perceived barriers to care as key factors limiting the
likelihood that ADF members would seek treatment for mental ill-health.[4]
A study investigating PTSD and stigma in the Australian Army, conducted by John
Bale for the Army in 2014, reported on Australian soldiers' experiences of stigma
due to mental ill-health. One solider commented:
After my break down and subsequent hospitalisation words
cannot express how lost I felt, the confusion and most of all the feeling of
despair. My Chain of command had no idea how to engage me and my unit turned
its back on me. Life was hard enough, but it was made harder that I had served
18 years and was not farewelled from my unit, mess, or Corps. It was not until
then that I realised that the stigma surrounding mental health and especially
PTSD within the Army was widespread.[5]
5.5
Another example told of a soldier being accused of malingering and his
concerns being dismissed when asking for mental health support and assistance from
members of his chain of command:
When first asking for assistance for mental health support
from within my immediate chain of command [sergeant and warrant officer class
2] I was met with an attitude that I was malingering and the immediate
questioning of my integrity as a JNCO.
I pursued the matter outside my chain of command, although
still within my unit, and a meeting with the unit RSM was arranged. I raised my
concerns about my mental health and wellbeing and was told to 'harden the f**k
up' and to get on with my job.[6]
5.6
The committee received similar evidence from ADF members and veterans
who told the committee that if ADF members raise concerns regarding mental
ill-health they are often dismissed or accused of malingering.[7]
Mr Matthew McKeever, a veteran, told the committee of his experiences, asserting
that ADF members who are struggling with mental ill-health, or even physically
injured, are commonly ostracised and called 'lingers':
As soon as they find out that you have a mental illness or
any kind of illness, regardless of whether it is a knee, back or whatever, you
are treated as a malingerer and you are treated quite badly. They do not want
to acknowledge you; they want to kick you out as soon as possible.[8]
You want to ask for help, but you know what the reaction is
going to be. I was a platoon sergeant. I used to sit in on med boards. I know
exactly what goes on in them. The words that are thrown around are, 'He's weak.
He is a linger. Let's just kick him out.' I have seen it firsthand because, as
a platoon sergeant, I am part of that criteria. I would quite often be spoken
down to because I would stand up for the soldier and say, 'No, that's not
right. He's got a serious injury.'
I had a soldier who, at 21, had a hip replacement. They just
booted him out of the army as a linger. That is not acceptable. They go on
about mateship, courage and initiative. Yes, courage and initiative is what you
have. Where does the mateship come into it? It does not.[9]
5.7
Dr Niall McLaren pointed to ADF cultural views of strength as a
significant contributing factor to the stigma surrounding mental ill-health:
Compounded in all of this is the intense stigma directed
against people with mental problems in the Defence forces, and this stems from
the myth of the 'real man'. The myth of the 'real man' is that there is no such
thing as pain, sickness or mental disorder, only weakness of will. Anybody who
shows pain, sickness or mental symptoms—and this is continuing with the myth—is
weak and must be treated harshly until he gets tough 'like us'. That myth is
absolutely rife. It is everywhere. It is in the air that people breathe in the
Defence forces. Of course, it is fantasy.[10]
5.8
The Chief of the Defence Force (CDF), Air Chief Mark Binskin, acknowledged
that stigma regarding mental ill-health is 'one of the biggest challenges we
continue to face in the Australian Defence Force'.[11]
However, when asked by the committee, the CDF disagreed with the allegations
that Defence had a cultural problem regarding members seeking assistance when
struggling with mental ill-health being ostracised and accused of malingering,
responding that 'No, I think that we have had issues in the past and I am sure
that there are pockets there now, still, that we will have to work on from a
cultural point of view for people to understand that this is a command issue in
looking to rehabilitate our people'.[12]
5.9
Defence assured the committee that it has introduced a range of
educational resources and activities to reduce stigma surrounding mental
ill-health:
...board developments and achievements since 2009
include...mental health education resources and activities such as the annual ADF
Mental Health Day to reduce stigma and barriers to care by increasing awareness
of mental health issues and understanding of PTSD, depression, suicide
prevention and alcohol misuse and how to seek help as early as possible.[13]
5.10
In the ADF Mental Health & Wellbeing Plan 2012-2015 (MHWP), Strategic
Objective 1 is 'to promote and support mental health fitness in the ADF' and
aims for:
-
a culture that promotes wellbeing and reduces the stigma and
barriers to mental health care;
-
ADF personnel who are mental health literate and know when, how,
and where to seek care for themselves and their peers; and
-
selection, training, and command systems that promote good mental
health and wellbeing.[14]
Impact of mental ill-health on
deployment and career
5.11
The MHWP study found that among its respondents, the highest rated
barrier to personnel seeking help for a 'stress-related, emotional, mental
health or family problem' in the ADF was the concern that seeking help would
reduce their deployability (36.9 per cent) and that seeking care would harm
their careers (26.9 per cent). This was also reflected in the evidence received
by the committee.[15]
5.12
Walking Wounded told the committee that the medical classification
system, and in particular, the requirement that Army personnel be able and
ready to deploy, reinforces and confirms ADF members' concerns that their
deployability is inextricably linked to their employability:
Most soldiers are honest but most soldiers are realists too.
Some years ago, when they changed the medical classification system in Army so
that you could no longer serve if you had an injury that prevented you from
serving overseas, that cut out a whole bunch of people who were very useful in
Army. Just because they could not deploy did not mean they
could not do good work elsewhere. I served many years ago with a major at
Kapooka, and it was not until I saw him running in PT gear that I realised he
only had one leg. He lost a leg in Vietnam thanks to a mine but he had
served—and this was 20 years after the end of Vietnam—quite happily with a
wooden leg. I thought: why not? Why would you want to lose that experience if
that person can still provide that service? We are not going to send him
overseas to fight again but, gee, there are lots of good jobs he could do in
Army otherwise.
Probably the greatest problem now is that the medical
classification system means that, if you are not ready to deploy, you cannot
continue employment in the Army. For a lot of young men and women that means
that they are losing the job they have always wanted. That is something that
needs to be addressed. When you are in uniform, you need that understanding
that the organisation is going to look after you, that it is going to keep you
on board and you have got that reassurance. Certainly when I was a digger that
was the case—you knew that you would certainly not be losing a job because you
had suffered a bad injury that you might not get back from. That is not the
case these days, of course.[16]
5.13
The Returned and Services League of Australia (RSL) stated that many ADF
members fear the impact that disclosing mental ill-health will have on their
ability to support their family:
Given a relative lack of civilian qualifications, many
servicemen/women (with mortgages and young families) fear the impact that
disclosing psychological injury will have on their ongoing employability,
deployability, promotional opportunities and therefore their incomes.[17]
5.14
Mr Mark Keynes told the committee:
Probably the biggest problem is the stigma associated with
seeking help. Many troops believe that anyone who asks for help is unlikely to
deploy and will probably be medically discharged. Many believe that asking for
help can be a career ending move, hence the stigma.[18]
5.15
Mr John Bale, in his report regarding PTSD and Stigma in the Australian
Army, highlighted ADF members' fears of being discharged as a key factor in
their reluctance to seek treatment for mental ill-health, especially for ADF
members of lower rank:
Job security is vital to soldiers. Soldiering is key to the
perceived self-worth of many who serve, and termination of employment by the
Army is a dramatic and often confronting experience and one that soldiers will
do almost anything to avoid. The fear of being discharged due to the disclosure
of PTSD is currently a significant barrier to care, and a promise made by the
senior leadership of the ADF and the Australian Army does little to reassure
the lower ranks of the Army who are among those most affected by PTSD.[19]
5.16
To allay these fears, Mr Bale called for the ADF to highlight positive
experiences from currently serving ADF members who have undergone
rehabilitation for mental ill-health and have successfully returned to their
career. Mr Bale also noted that this will also encourage ADF members to seek
treatment early, to improve their chances of successful rehabilitation:
The most effective way to allay fears over job security for
those who seek treatment for PTSD is to highlight positive experiences from
currently serving soldiers who have been rehabilitated and subsequently enjoyed
successful careers. These soldiers' stories, highlighting their successful
return to an Army career, present a highly effective means of reassuring those
with PTSD that they will only be medically discharged if they cannot be
successfully rehabilitated. This message can also be useful in reinforcing the
need for early intervention, signalling the fact that the sooner individual
sufferers seek help, the greater the chance of their recovery, and the less
likely they are to face discharge.[20]
5.17
Defence emphasised its commitment to rehabilitation, informing the
committee that of the 869 individuals with a mental illness who completed a
rehabilitation program in the period from July 2013 to June 2014 a total of 420
(or 52 per cent) are recorded as having a successful return to work at the end
of their rehabilitation program. Defence provided three recent examples of ADF
members of differing ranks that completed a rehabilitation program following referral
for mental illness:
The first example involves an officer who was diagnosed with
PTSD following an operational deployment in 2011. The officer’s health care and
rehabilitation program included a six week PTSD program. The officer was
successfully returned to work in his current unit. As at October 2015, it is
reported that the officer remains well supported by his unit and colleagues,
and his ongoing prognosis and needs are being monitored by his health care
team.
The second example involves a Senior Non Commissioned Officer
(SNCO) who was medically downgraded because of both physical and mental health
conditions related to multiple deployments. During 2014, the SNCO was provided
with clinical treatment and health care, and referred to the ADF Rehabilitation
Program. With the support of the rehabilitation consultant, commanding officer
and health care team, the SNCO remained in the unit and was given the time to
recover and achieve a full return to work outcome. The SNCO was medically
upgraded in mid 2015, is undertaking a military course and will potentially be
posted and deployed again in 2016.
The third example involves a junior ranked soldier with
specialist skills who witnessed deaths during multiple deployments, resulting
in a mental health condition. This member was provided with health care and
referred for rehabilitation during 2013. The rehabilitation was successful,
with the member being medically upgraded, promoted to a Non Commissioned
Officer (NCO), and deployed on operation again in 2014.[21]
5.18
The RSL also commended the ADF, noting the 'great step forward' of
providing a mandatory two-year period of treatment, rehabilitation and/or
vocational training for ADF members allowing members to adapt their career
plans:
The ADF's recent initiative of giving their employees a
mandatory 2 year period of treatment/rehabilitation/vocational training (either
back into ADF employment or in the civilian world) once a significant injury is
identified is a great step forward.[22]
5.19
Defence developed a 30-minute documentary, Dents in the Soul–helping
to cope with PTSD, which is available from the Defence Health portal
website. The documentary aims to 'de-stigmatise PTSD and to show that it can
potentially happen to anyone'. It acknowledges ADF members' fears of stigma and
condemns attitudes that mental ill-health is 'weakness'. The documentary calls
for 'psychological sentry duty' asserting that commanders and fellow ADF
members have a duty to look out for and to help anyone struggling with mental
ill-health and declaring that those who do not have failed their subordinates
or their mates.[23]
The documentary features interviews with current ADF members who have undergone
successful rehabilitation for PTSD and returned to work, emphasising that
'recovery rates from PTSD are high but early diagnosis and treatment are
particularly important'. It strongly and repeatedly emphasises that Defence has
invested in and values ADF members and states its desire to rehabilitate and
retain its members.[24]
5.20
Aspen Medical reported that 42 per cent of its clinicians agreed or
strongly agreed with the statement that there is increasing awareness and
acceptance of mental health issues and PTSD amongst Defence personnel which is
reducing the stigma formerly attached to mental health issues, with 21 per cent
disagreeing or strongly disagreeing. Aspen Medical commented that 'this
suggests that attitudes are changing within the ADF and that the efforts of the
ADF and JHC have met with some success', as well as noting that 'it is also
clear that this cultural shift will take more time to become fully embedded
within the ADF'.[25]
Department of Veterans' Affairs claims processes
5.21
DVA is responsible for a range of programs providing 'care,
compensation, income support, and commemoration for the veteran and defence
force communities and their families'. DVA administers three key pieces of
legislation which governs veterans access to care and support entitlements:
-
Veterans Entitlements Act 1986 (VEA), which provides
compensation, income support, and health services for those current and former
members of the ADF who have rendered services in wars, conflicts, peacekeeping
operations, and certain other deployments before 30 June 2004. Current and
former ADF members with peacetime service between 1972 and 1994 and some
veterans with warlike service and non-warlike service after 1 July 2004 may
also have access to certain VEA entitlements;
-
Safety, Rehabilitation and Compensation Act 1988 (SRCA),
which is workers' compensation legislation that applied to members and former
members of the ADF, Reservists, Cadets, and Cadet Instructors and certain other
persons who hold an honorary rank in the ADF, as well as members of certain
philanthropic organisations that provide services to the ADF; and
-
Military Rehabilitation and Compensation Act 2004 (MRCA),
which provides compensation and rehabilitation for current and former members
of the ADF as well as Cadets, Cadet Officers, and Instructors whose injury or
disease is caused by service on or after 1 July 2004. The MRCA superseded the
SRCA at this date for DVA, as well as most of the provisions contained within
the VEA.[26]
5.22
There are two ways that veterans can apply to DVA for assistance with
mental health conditions:
-
the non-liability pathway: for certain mental health conditions
whatever the cause, to receive treatment only; and
-
the liability pathway: for mental health conditions related to
service in the ADF, to receive compensation and treatment.[27]
Non-liability pathway
5.23
In 2013, DVA approved 1,244 non-liability applications for mental health
and in 2014, approved 3,826.[28]
DVA advised the committee that the eligibility requirements for non-liability
mental health service provision were expanded in 2014 and again in 2015.
Non-liability mental health services are now available to anyone who has
deployed on operations overseas or has completed three or more years of
continuous service in peacetime since 1972.[29]
5.24
Under the new arrangements, DVA can pay for treatment for diagnosed
PTSD, anxiety, depression, alcohol use disorder, or substance use disorder
whatever the cause. Furthermore, DVA can now accept diagnosis from vocationally
registered GPs, clinical psychologists, or psychiatrists. If a person has been
diagnosed with one or more of these conditions, they are issued with a White
Treatment Card (White Card), which provides access to treatment such as GP
care; specialist care in the community, such as from a psychologist or
psychiatrist; and hospital care.[30]
5.25
A number of submissions supported non-liability mental health service
provision and called for eligibility to be broadened further.[31]
The RSL described the provision of non-liability support as 'invaluable' but
called for eligibility to be extended to everyone who has served in the ADF:
DVA's non-liability mental health support for eligible
veterans has proved to be invaluable for the veterans who often present to an
RSL Pension Officer at breaking point. This allows them to immediately access
specialist health while their DVA claim is processed. The RSL
would support the extension of non-liability mental health support to all who
have served in the ADF.[32]
Liability pathway
5.26
A serving or ex-serving ADF member who has a medical condition,
including mental health conditions, for reasons related to their service, can
make a liability claim. Once the liability claim has been accepted, DVA can
provide services such as rehabilitation (including vocational assistance),
medical treatment, (such as White or Gold Treatment Cards), attendant care, household
services, and a range of other benefits. Compensation may also be provided for
an inability or reduced ability to work or to recognise the effects of a
permanent impairment resulting from a service-related incident.[33]
5.27
DVA assesses claims to determine whether the injury, illness, or disease
is related to the claimant's service, with most claims being assessed under the
VEA, SRCA or MRCA, depending on which piece of legislation applies to the
claimant. Claims processed under the VEA or MRCA are assessed using Statements
of Principles, which list factors that 'must' or 'must as a minimum' exist to
cause a particular kind of disease, injury or death and which could be related
to military service. The Statements of Principles are determined by the Repatriation
Medical Authority, which consists of a panel of practitioners eminent in fields
of medical science. Claims processed under the SRCA are assessed 'using
available medical evidence to support consideration of a disease, injury, or
illness'.[34]
Impact of claims processes on
mental health of claimants and their families
5.28
The committee received considerable evidence regarding the difficulties
that many veterans, especially those struggling with mental ill-health, have
when seeking assistance from DVA, and the detrimental impact that the claims
process can have on their mental health.[35]
The RSL told the committee that 'the DVA Compensation process complicates,
aggravates and perpetuates the pre-existing psychological distress suffered by
veterans and their families'.[36]
5.29
Slater & Gordon Lawyers described the DVA claims process as
'combative' noting that its clients' experiences with the DVA claims process
are detrimental to their already compromised mental health:
We are witnessing Veterans being drawn into a system of
combative legislation with a bureaucracy of Departments shifting
responsibility. My team can attest to the voices of other Veterans advocates
and ex-service organisations that lodging claims with the DVA for compensation
and treatment of physical and mental issues is "like going through a meat
grinder, it grinds you up".[37]
5.30
Soldier On highlighted the confusing and overwhelming nature of the DVA
claims processes, noting that it 'routinely aggravates existing mental health
conditions':
The process of navigating a claims process routinely
aggravates existing mental health concerns in many people attempting to access
support from DVA. One partner of a veteran said they weren't in a position to
sit down and manage their way through the confusing mix of support available.
She described it as looking at the night sky. "There are many bright,
shiny places to go, but out of the hundreds of options, where are we meant to
go? What we need is a map, we don't need more stars."[38]
5.31
Mrs Catherine Lawler, the wife of a veteran struggling with mental
ill-health, told the committee that the claims process can be overwhelming for
both veterans and their families. Mrs Lawler noted that the 'torturous and
arduous' claims process results in many veterans giving up on their claim:
...lodging a claim with DVA may seem to be a reasonable
straight forward process, but the legal aspects under consideration are
complex, potentially involving multiple pieces of legislation, the
administrative requirements exacting, and the time frames very lengthy. And the
veteran is expected to deal with all of this while living with the debilitating
effects of PTSD or mental illness.
It is a torturous and arduous process that serves only to
increase the stress levels of the veteran and it impacts negatively on them and
their family. The distress generated frequently becomes too much for the
veteran, and they give up on their claim, walk away from their family, or take
their own lives. There is no support within this process for the partners or
families of veterans with PTSD or mental illness.[39]
Criticisms of DVA's delivery models
and claims processes
5.32
In 2013, the Australian Public Service Commission conducted a capability
review of DVA. The review found that 'DVA staff are committed to supporting the
Australian veteran community' but that 'a major transformational leap forward
is required'.[40]
The capability review expressed serious concerns regarding DVA's delivery
models and compensation claims processing:
DVA’s current operating structure is a complex matrix—an
unsustainable hybrid of fragmented national and dispersed business lines,
comprising multiple service models, much of which is delivered and processed
in-house (with the exception of health services which is outsourced).
This complexity has partially been shaped by the combination
of multi-act eligibility and an increase in claims made under the MRCA which is
more challenging to administer, but primarily through the division of
responsibility for staff, policy and service delivery, all of which can be
split across two or three divisions and two or more locations. This complex
structure lacks scale and has contributed to the development of fiefdoms in
state locations and functional silos to the detriment of consistency and
efficiency of performance across key business outcomes, particularly
compensation claims processing.[41]
5.33
Mr Brian Briggs, Practice Group Leader, Military Compensation, at Slater
& Gordon Lawyers described the DVA claims processes as 'chaotic'
identifying 'fundamental problems' with its culture, leadership and equipment:
My first suggestion is this simple proposition: tackle the
chaotic claims handling by DVA. An Australian Public Service Commission review
found that the Department of Veterans’ Affairs has fundamental problems with
its culture, leadership and equipment. The department has itself admitted that
it cannot deal with the complicated needs of many physically and mentally
injured veterans. The APSC review further found that the decision-making
process at Veterans’ Affairs was a confusing mess of committees with duplicated
membership and overlapping agendas. For example, 200 individual ICT systems
operating within a single department cannot be efficient or productive. The
structure of small cells of public servants working in isolation and not
considering the whole picture has failed. Files are shipped all over the
country—one section may deal with liability before another considers incapacity
and then another rehabilitation or treatment. Permanent impairment and
compensation will be looked at by an entirely separate team. This entire
bureaucratic file shuffling and passing on of an injured member's claim causes
significant delays. The frustration of my clients at this inefficiency and
ineptitude often overwhelms.[42]
5.34
DVA emphasised its desire to improve its engagement with clients,
advising the committee that in late 2014, it commissioned and independent
survey to help improve client services which collected approximately 3,000
responses. The results showed that 89 per cent of clients were satisfied with
DVA's client service and 90 per cent of clients 'believed that the Department
is honest and ethical in its dealings and is committed to providing high
quality client service'.[43]
5.35
Mr Shane Carmody, the Chief Operating Officer of DVA, acknowledged both
the findings of the Capability Review and the comments made by Mr Briggs,
assuring the committee that DVA has strategies in place to address DVA's
operating structure; governance arrangements; information and communications
technology; approach to clients; culture and staffing; and its efforts to
formulate effective strategy, establish priorities, and use feedback:
The review team identified three key areas of focus, and we
have discussed those I think more than once during the estimates process. They
saw that we needed urgent attention to transforming our operating structure;
our governance arrangements and information and communications technology; our
approach to clients, culture and staffing; and our efforts to formulate
effective strategy, establish priorities and use feedback. All of these issues
have been identified, and strategies are in place to deal with them through
DVA's strategic plan towards 2020.
In terms of operating structure, as we mentioned during a
number of hearings, part of the creation of my position as chief operating
officer was to streamline the governance process and take control of a number
of key aspects of business. We have programs underway in terms of our clients,
culture and staffing, including a strong program such as 'It's why we're here',
a very clear program to ensure that our staff have a very good understanding of
the client base we are dealing with and the injuries and illnesses they face.[44]
Complex application processes
5.36
A number of submissions highlighted the complex and confusing
applications processes required to lodge a claim.[45]
The RSL acknowledged that DVA's 'strict processes are required to efficiently
and fairly investigate large number of claims' and that DVA has 'a defined
budget' within which it must operate but noted that this has led to an
adversarial system where DVA's focus appears to have shifted from supporting
veterans to 'looking for reasons not to provide compensation':
...many veterans feel that they are viewed by DVA as trying to
cheat the system until proven otherwise. The majority of veterans and advocates
(with whom the RSL and other advocates have contact) relate that a steadily
increasing proportion of claims seem to be proceeding to the Veterans Review
Board and the Administrative Appeals Tribunal, which indicates that the DVA is
looking for reasons not to provide compensation rather than ways to support
their clients.[46]
5.37
Mr William Kearney, from the Wide Bay Burnett District of the RSL, told
the committee that most veterans, and even many volunteer advocates, do not
understand the complex legalities of the claims process and highlighted the
significant consequences for veterans and dependants if they, or the volunteer
advocates assisting them, are unable to correctly navigate the system:
The danger here is that well meant but incorrect advice, once
put on a form, signed by the applicant, then submitted to the Department is
evidence that cannot be undone. Further clarification may have a
slim chance of repairing damage but this is extremely rare. The outcome of this
is that a Veteran, at best, is locked into a lengthy appeals process, or
alternately denied benefits for life that they could have been receiving if the
case was done correctly.[47]
5.38
DVA advised the committee that it has 'invested significantly' in its
online capacity and improving clients' experiences with the claims processes.
Clients can access online claiming for a range of DVA claims and applications,
including claims for 'liability compensation following the death of a veteran, determining
qualifying service, and service pension and income support supplement'.
Furthermore, DVA advised that it has introduced an online 'single claim
process' which negates the need for clients to make separate claims under
different pieces of legislation:
The online claiming process is a single claim process rather
than the client needing to make separate claims under different pieces of
legislation. Claims will be considered under all relevant legislation to ensure
clients have access to the full range of benefits for which they are eligible.
The feedback received from ex-service representatives and departmental staff
following a trial clearly showed that a single claim form is far less complex
for clients.[48]
5.39
The DVA website now also offers a range of services including
'Entitlement Self-Assessment', which comprises a series of questions to help
existing and prospective DVA clients to assess their potential entitlements.
This may be completed by a member or former member of the ADF, (including
reservists and cadets) or dependants (partner/spouse or children). Clients can
also access 'my Account', which allows clients to access a range of DVA
services online. Clients can update contact details, access information about
accepted medical conditions, make transport bookings, claim travel expenses,
and access forms and fact sheets.[49]
Recordkeeping, communications
technology, and procedural errors
5.40
The committee received evidence regarding lost documents, long delays
whilst waiting for documents to be physically transferred between offices, and procedural
errors.[50]
Soldier On told the committee that veterans have told them of documents being
lost by DVA:
When we have spoken to a number of veterans it seems that
sometimes their records are either lost or they are not handed over correctly.
When you have a mental health injury, actually talking through the same thing
again and again can be quite confronting, especially when you have to relive
your wound. So, for whatever reason it seems that records are not passed on
correctly. That may mean they are kept correctly but not passed on correctly.[51]
5.41
One submitter told the committee that confidential medical documents
were lost by DVA on multiple occasions and outlined a number of procedural and
clerical errors that were made by DVA over the two years it took for their husband's
claim to be finalised:
Documents including confidential medical documents were lost
on more than one occasion, and requests for responses to emails, phone calls
and letters were consistently ignored. Months would pass without any updates to
the claim, despite repeated requests for information.
A number of procedural mistakes and errors of judgement
occurred during the course of the claim including:
-
the date of onset of the illness being determined incorrectly (there was
a 7 year difference)
-
not receiving the White Card for treatment costs until after liability
was established
-
not being assessed for rehabilitation services despite requests for
these services
-
the level of permanent impairment points determined by DVA was
overturned on appeal by the Veterans Review Board (VRB)
-
the procedures for determining the payment period for Incapacity
Payments were found to be incorrect and also overturned on appeal by the VRB.[52]
ICT systems
5.42
The capability review identified the state of DVA's ICT systems as a
significant issue to be addressed, describing the systems as 'antiquated':
...the department is delivering through some 200 ICT systems
which are so antiquated that new staff feel they have been transported back ‘10
years or more’. Applications are not integrated, making it difficult to obtain
a whole-of-client perspective. This is further affected by a lack of a single
client identification either within DVA or flowing from Defence through to DVA.
Past investment has been a patchwork in the absence of a definitive ICT
blueprint, which has generated cynicism and frustration.[53]
5.43
Mr Carmody agreed that DVA has 'antiquated' ICT systems, assuring the
committee that DVA was working to modernise and digitise its systems 'within
the funding' available:
We do have challenges—I will admit those—without a doubt. I
mentioned some during a hearing last week. We have antiquated ICT systems. We
are doing our best to modernise those systems within the funding that we have
available. We are doing our best to digitise our systems to move files off
paper and on to digital systems. It will take time.[54]
Case coordination
5.44
A number of submissions highlighted the lack of continuity when dealing
with DVA and called for veterans making claims regarding mental ill-health to
be assigned a case officer or staff member to act as a single point of contact.[55]
One submitter called for DVA to assign a case officer to act as a single point
of contact for claims relating to mental ill-health:
Each time we contacted DVA we would speak with a different
staff member, who inevitably passed us on to someone else, usually in another
state. A dedicated case manager, with specialist training in mental health
awareness should be allocated to each case that involves mental illness.[56]
5.45
DVA advised the committee that a small proportion of DVA clients are categorised
as 'vulnerable with complex needs'. This might be because the client has
serious wounds, illnesses, or injuries as a result of their service; a severe
mental health condition; relationship or interpersonal difficulties; complex
psychosocial needs; or a mix or some of all of these factors. DVA noted that,
in general, case management refers to support provided to clients for:
-
access to DVA systems and supports, usually referred to as 'case
coordination', which are provided through DVA's case coordination service; and
-
access to health care and community service, usually referred to
as 'clinical care coordination', which are provided through DVA's health care
card arrangements (for instance, through social workers) and also through the
Veterans and Veterans Families Counselling Service (VVCS).[57]
5.46
DVA informed the committee that in the 2015-16 budget, the government
funded 'a new measure', worth approximately $10 million over the forward
estimates, to improve DVA's case coordination:
The measure will improve DVA's capacity to provide one-on-one
tailored packages of support to veterans with complex needs, including mental
health conditions. It will also improve the level of support and early
intervention assistance provided to an increasing number of veterans with
complex needs, particularly those returning from recent conflicts.[58]
5.47
Furthermore, as of 8 February 2016, DVA has implemented a single,
nationally consistent, model for supporting complex and multiple needs clients.
DVA advised that the new model focuses on supporting clients with mental health
conditions and/or complex needs and aims to provide a single point of contact:
In line with the aim of the Budget initiative, there is a
focus on supporting clients with mental health conditions and/or complex
needs. Staff working within the new model will provide a single point of
contact where appropriate, help clients navigate DVA’s processes to ensure they
are accessing all of their entitlements, and connect clients with other
community-based services and support where relevant.[59]
5.48
DVA also provided data regarding client update of the various case
management support options (see table 5.1).
Table 5.1–Client update of case
management support
|
Program/Support
|
Data on client uptake or population*
|
|
DVA’s case coordination service
This is a single service providing those clients requiring
additional support with a primary or single point of contact for the whole of
the Department.
|
From January 2010 to June 2015, over 1,100 clients were
referred to the Case Coordination Program.
As part of the information exchange strategy between Defence
and DVA, in 2014-2015 Defence issued DVA with:
17 NOTICAS* priority notifications; and
961 medical separation notifications.
*Where a member is medically classified as seriously or very
seriously wounded, injured, or ill (defined as an injury or illness that
endangers the person’s life; significantly disables the person; or materially
affects the person’s future life).
|
|
Social work services under DVA’s allied health
arrangements
Social workers help clients overcome a range of problems in
relation to stressful life events such as death or divorce and assist them to
deal with family, health, employment, income support or accommodation related
issues. The services provided by eligible social workers may include:
-
general counselling and case management; and
-
health service co-ordination and facilitating access to
community services.
|
In 2014-15, there were 906 clients who received support under
DVA’s social work allied health items, for treatment or case coordination.
|
|
Veterans and Veterans Families Counselling Service (VVCS)
VVCS provides free and confidential, nation-wide counselling
and support for war and service-related mental health conditions, such as
posttraumatic stress disorder (PTSD), anxiety, depression, sleep disturbance
and anger.
VVCS supports a number of clients in complex situations with
comorbidities and or who find it difficult to engage and manage the range of
health and social care services they require.
|
In 2014-15, there were 227 clients who had their cases
managed by VVCS. This compares with 126 complex care cases managed
in 2013-14.
|
* Note: the same client may
access more than one type of support.
Department of Veterans'
Affairs, Supplementary Submission 35.1, pp 2–3.
Timeframes
5.49
A number of submissions raised concerns regarding the time taken to
process claims.[60]
Slater & Gordon Lawyers and KCI Lawyers called for the introduction of time
limits for the processing of claims. Slater & Gordon Lawyers noted that
state and territory bodies as well as international bodies have statutory
timeframes in which decisions are made regarding the processing of claims for
assistance and compensation:
...most important, is that time frames are now put in place to
ensure that claims for help and other things are dealt with. Every state and
territory system in Australia has time frames for decision making. Defence
personnel in the UK and US are protected by time frames for decision making.
But in Australia there are none, so injured personnel can literally be left
waiting for years...An increase of $10 million announced in the latest budget to
increase the numbers of delegates who make decisions is welcome but will not
adequately solve the problem unless time frames are mandated. I strongly urge the
committee to consider the issue of deeming time periods, which will have a
significant benefit in assisting not only the PDSD sufferers but also all of
our injured military personnel.[61]
5.50
KCI Lawyers commented that the long processing times unfairly deny veterans
and their families access to much needed assistance:
DVA continue to cause Veterans and their families substantial
delays as they have no time limits imposed to make timely decisions. This
remains a vexed issue when compared to other Workers' compensation...The time has
well and truly come for DVA to make a decision within a reasonable and a
defined period. The old adage of "justice delayed is justice denied"
is also true when considering the delay to provide compensation payments by
making timely and accurate decisions is akin to denying the benefit.[62]
5.51
DVA assured the committee that 'the Government is very focussed on
improvements to reduce the time taken to process compensation claims'
describing it as a 'key early intervention initiative'.[63]
The average times taken to process compensation claims under the VEA and
liability claims under MRCA and SRCA for the financial years 2011-12 to 2013-14
are listed in table 5.2.
Table 5.2 – Time taken to process
claims
|
|
TARGET AVERAGE
days
|
2011-12 OUTCOME
days
|
2012-13 OUTCOME
days
|
2013-14 OUTCOME
days
|
2013-14 CHANGE
days
|
|
VEA
|
75
|
74
|
79
|
75
|
-4
|
|
MRCA
|
120
|
158
|
155
|
144
|
-11
|
|
SRCA
|
120
|
180
|
171
|
160
|
-11
|
Department of Veterans'
Affairs, Submission 35, p. 28.
5.52
DVA disagreed with calls to introduce statutory timeframes. Ms Lisa
Foreman, First Assistant Secretary, Rehabilitation and Support, advised the
committee that statutory timeframes have been considered in the past and were
found to be unsuitable for DVA's unique situation:
Last year, we tabled a report in the Senate on the review of
statutory time frames which looked at the options that we might be able to
adopt in relation to our claims processes, but overall there are two
significant issues in relation to compensation claims that we receive compared
to compensation claims under states' compensation and private compensation
schemes. Firstly, we have no time limit on when a member—a veteran—can lodge a
claim. So an injury could have occurred in the forties, the fifties or the
sixties, and a veteran is still able to lodge a claim with us; there is no
limit. We do not have any directions on the state of the
claim that we receive. Essentially, a veteran can put a claim in which just has
their name, address and injury, and they sign it. A lot of other compensation
schemes actually will not accept a claim until it is fully completed. In our
case, that would mean that it has not only the details of the veteran but also
reports from their medical specialists or doctors about the nature of the
injury and the illness, proof of identity that the veteran has served, and
details of where they served and when they served. We do not do that; we allow
veterans to come in and immediately give us their claims. We then go away and
try and get that additional information. We will contact their specialists and
ask them to produce a report. We will contact Defence and ask them to produce
details of their medical records and the incident that gave rise to the
compensation. I think, overall, we are in a very different position to other
compensation schemes in Australia.[64]
5.53
Mr Carmody also expressed concerns regarding the introduction of
statutory timeframes, noting that it could damage the integrity of the claims
system:
...one of the key points in statutory time frames is what you
wish to achieve. For example, do you want to have a deemed acceptance at the
end of a particular period? If that were the case, that would encourage
everybody to go slow on their claims process, because we have to collect all of
the information. If you were to have a deemed acceptance, people would be
reluctant to put in their material, because at the end of a particular period
of time we are going to accept it anyway. That would be unfair across the whole
system. If you decided to have a deemed rejection at the end of a particular
period, if somebody gets 95 per cent through their claims process and the time
elapses, they have to go back and start again. So there are some real issues in
trying to manage this. A great amount of our time that is taken to process is
taken up with collecting information which in other jurisdictions would be
provided in advance. That is probably the simplest answer.[65]
Availability of services in regional and remote areas
5.54
Some submissions highlighted a lack of available services, especially in
regional or remote areas, as a significant barrier to treatment.[66]
Ms Maria Brett, Chief Executive Officer of Psychotherapy and Counselling
Federation of Australia, told the committee that due to workforce shortages,
veterans seeking treatment may have to wait a 'significant amount of time':
...particularly relates to rural and regional areas, because we
know there are workforce shortages. If you are trying to access one of the
outreach counsellors from VVCS and you live in a place where someone is not
available, you will actually be waiting, and that sometimes can be for quite a
significant amount of time to get a service. This is why, in our discussions
with the health minister we are very interested in potentially using
counsellors to participate in a rural and regional trial, and that could be
something potentially that DVA—[67]
5.55
Ms Catherine O'Toole, Chief Executive Officer at Supported Options in
Lifestyle & Access Services (SOLAS), advised the committee that 'specialist
mental health services are very light on the ground in regional areas'. Ms
O'Toole advised that SOLAS was working to build capacity in northern and
western Queensland:
Specialist mental health services are very light on the
ground in regional areas. Our organisation made a commitment, when we got
federal funding some time ago, that we would work to build the capacity in our
regional areas. That is why we subcontract in Charters Towers, Ingham, Ayr,
Burdekin, Richmond and Hughenden—because there were no specialist mental health
services. We have been able to build that capacity in that community. It is
much more financially viable as well. We have also created jobs and built skill
bases in those communities.[68]
5.56
DVA acknowledged that, as it operates and purchases services from within
the broader mental health system, workforce shortages can impact on the
availability of services for veterans in regional and remote areas:
DVA operates within a broader mental health system and it is
important to recognise that while there has been significant expansion of
mental health services over the past two decades in Australia, this sector
continues to have workforce shortages in the face of growing demand especially
in some regional areas.[69]
Committee view
Stigma and perceived barriers to
care
5.57
Early identification and treatment of mental ill-health is essential for
achieving the best outcomes for ADF members and veterans with mental
ill-health. As such, the committee is very concerned that perceived stigma
surrounding mental ill-health continues to be identified as a significant
barrier to ADF members and veterans seeking treatment for mental ill-health.
5.58
Evidence of ADF members who were brave enough to report mental
ill-health and seek treatment being ostracised, ridiculed, and accused of
'malingering' is deeply disturbing and completely unacceptable. The committee
acknowledges that Defence has introduced a range of educational resources and
activities to reduce stigma surrounding mental health; however, it is clear
that more must be done to root out and denounce stigma regarding mental
ill-health.
Impact of mental health on career
prospects
5.59
The MHWP study found that the highest rated barrier to ADF personnel
seeking help was the concern that seeking help would reduce their deployability
(36.9 per cent). The committee acknowledges that is a legitimate fear and a
difficult one for Defence to address. Defence has an obligation to ensure that
ADF member's duties do not detrimentally affect their health, that ADF members
can undertake their duties without compromising the safety of themselves or
others, and that the ADF as a whole maintains it operational capability.
5.60
The committee understands the principle that it would be inappropriate and
irresponsible for Defence to deploy ADF members who are not mentally well
enough for deployment, in the same way as it would be inappropriate for an ADF
member who is not physically well enough to be deployed. However, this does not
absolve Defence of its responsibility to address these fears. Defence should
continue to emphasise the benefit of early identification and treatment of
mental ill-health for an ADF members' long-term career prospects when
considering seeking assistance for mental ill-health. Defence should also encourage
ADF members to plan beyond their next deployment by showing examples of members
who have successfully deployed after rehabilitation for mental ill-health.
5.61
An ADF member who chooses not to disclose or treat mental ill-health,
and is subsequently deployed, is exposing themselves to significant risk of
further deterioration of their mental health. This may result in a much more
serious mental health condition which may ultimately lead to the ADF member
being medically downgraded, medically discharged, or even the inability to work
at all. Comparatively, an ADF member who disclosed and sought treatment for
mental ill-health early may have their deployment delayed, but is significantly
more likely to have positive mental health outcomes. This may result in later
deployments, after mental health concerns have been addressed, and ultimately
result in a longer and more successful career in the ADF.
Recommendation 11
5.62
The committee recommends that Defence mental health awareness programs do
more to emphasise the benefit of early identification and treatment of mental
ill-health for an ADF members' long-term career and encourage ADF members to plan
beyond their next deployment.
Recommendation 12
5.63
The committee recommends that the Department of Defence and the
Department of Veterans' Affairs develop a program to engage current and former
ADF members, who have successfully deployed after rehabilitation for mental
ill-health, to be 'mental health champions' to assist in the
de-stigmatisation of mental ill-health.
DVA delivery models, claims
processes, and ICT systems
5.64
Veterans and their families who are seeking assistance and treatment for
mental ill-health must engage with DVA to receive it. Therefore, the extent to
which DVA processes act as a barrier to the early identification and treatment
of mental ill-health is directly proportionate to the ease and speed with which
veterans' claims are processed. As such, the committee is deeply concerned by
evidence that the DVA claims process can be detrimental to the mental health of
veterans seeking assistance and treatment for mental ill-health.
5.65
The Australian Public Service Commission's capability review highlighted
considerable failings regarding DVA's operating structure; governance
arrangements; information and communications technology; approach to clients;
culture and staffing; and its ability to formulate effective strategy,
establish priorities and use feedback. The committee acknowledges that DVA has
strategies in place to address these shortcomings; however, it is clear that more
must be done to ensure that veterans are able to quickly access the assistance
and treatment they require.
5.66
The committee commends DVA for its efforts to simplify its complex claims
process. The introduction of an online 'single claims process', which negates
the need for clients to make separate claims under different pieces of
legislation and ensuring that clients have access to the full range of benefits
that they are eligible for, is a significant step towards improving client
engagement. The committee also notes DVA's introduction of online 'entitlement
self-assessment' and 'my Account' services.
5.67
The committee is very concerned by the evidence it received regarding
lost documents, long delays whilst waiting for documents to be physically
transferred between offices across different states and territories, and
procedural errors. DVA's 'antiquated' ICT systems appear to be at the root of
many of these concerns. The committee is not satisfied by DVA's comments that
'it will take time' to modernise these systems within the funding that it has
available. The digitisation of records and modernisation of ICT systems must be
made a priority and should be funded accordingly.
Recommendation 13
5.68
The committee recommends that the Department of Veterans' Affairs be
adequately funded to achieve a full digitisation of its records and modernisation
of its ICT systems by 2020, including the introduction of a single coherent
system to process and manage claims.
5.69
Good case coordination is essential to ensuring that veterans and their
families who are seeking assistance for mental ill-health can navigate the
claims process with the minimum impact on their mental health. The committee is
satisfied that DVA recognises this and is encouraged by the government's recent
investment to improve DVA's case coordination. The committee is also pleased to
note DVA's recent implementation of a single, nationally consistent, model for
supporting complex and multiple needs clients, which will aim to provide a
single point of contact during the claims process.
5.70
Early identification and treatment of mental ill-health is essential for
achieving the best outcomes for ADF members and veterans with mental
ill-health. As such, it is essential that claims are processed in a timely
fashion, to ensure that veterans and their families are able to receive
assistance and treatment as soon as possible. The committee commends DVA for
its non-liability mental healthcare provision and its recent expansions to the
eligibility requirements to receive it.
5.71
The committee acknowledges DVA's assurances that it is aware of the
importance of improving the timeliness of claims processing. The committee is
satisfied that the strategies DVA is implementing to improve the timeliness of
its claims processing, together with the digitisation of records and
modernisation of ICT systems, will ensure that claims are processed within
acceptable timeframes.
5.72
The committee acknowledges calls to introduce statutory timeframes;
however, based on the evidence received, the committee is not convinced that
mandating a timeframe will benefit veterans and may have unintended
consequences.
Navigation: Previous Page | Contents | Next Page