Introduction
1.1
The aged care sector has experienced the impacts of significant changes
in recent years. These changes range from the ageing of the Australian
population and the corresponding ageing of the workforce, the increased use of
technology in service delivery, the increased complexity of health needs of
individuals entering aged care, and the shift in policy approaches to aged
care, with much service delivery now occurring at home to allow people to 'age
in place' for longer rather than enter institutions at the first sign of
age-related frailty. All of these developments are placing significant pressure
on the aged care workforce.
1.2
At the same time, the funding model for aged care has shifted from a
model where service delivery organisations were directly funded by government
through 'block funding', to a market-based model, where consumers of services exercise
greater control over how funding is spent. In this new approach, eligible individuals
are largely able to choose for themselves what services they need and the
organisations or individuals they wish to deliver those services, via the new
Consumer Directed Care (CDC) model of service delivery.
1.3
A similar change to disability service funding, via the introduction of
the National Disability Insurance Scheme (NDIS), has also seen impacts in the
disability sector. In addition, the rollout of the NDIS adds to pressures on
the aged care workforce as the need for more staff grows across both the disability
and aged care sectors.
1.4
The focus of this inquiry has been to ensure scrutiny is also placed on
the aged care service sector, which, like the disability service sector, is
responsible for the direct care of vulnerable Australians. This inquiry was
undertaken to review the current frameworks under which aged care providers
recruit, train and retain their workforce, and to anticipate the impact of
current and expected changes to the aged care service sector, and the workforce
which will be needed to deliver those services in the years to come.
Terms of reference
1.5
The terms of reference for this inquiry are:
- the current composition of the aged care workforce;
- future aged care workforce requirements, including the impacts of sector
growth, changes in how care is delivered, and increasing competition for
workers;
- the interaction of aged care workforce needs with employment by the
broader community services sector, including workforce needs in disability,
health and other areas, and increased employment as the National Disability
Insurance Scheme rolls out;
- challenges in attracting and retaining aged care workers;
- factors impacting aged care workers, including remuneration, working
environment, staffing ratios, education and training, skills development and
career paths;
- the role and regulation of registered training organisations, including
work placements, and the quality and consistency of qualifications awarded;
- government policies at the state, territory and Commonwealth level which
have a significant impact on the aged care workforce;
- relevant parallels or strategies in an international context;
- the role of government in providing a coordinated strategic approach for
the sector;
- challenges of creating a culturally competent and inclusive aged care
workforce to cater for the different care needs of Aboriginal and Torres Strait
Islander peoples, culturally and linguistically diverse groups and lesbian,
gay, bisexual, transgender and intersex people;
- the particular aged care workforce challenges in regional towns and
remote communities;
- impact of the Government's cuts to the Aged Care Workforce Fund; and
- any other related matters.
Report structure
1.6
This report is divided into five chapters:
-
Chapter 1 provides a background to the committee's inquiry
and an overview of the changing Australian aged care sector and the composition
of the workforce. The chapter also reviews the role of government in developing
workforce strategies.
-
Chapter 2 examines the changing environment in which the
aged care workforce operates, including new service delivery models, increasing
use of technology and the increasingly complex needs of people entering the
aged care system.
-
Chapter 3 examines the challenges in attracting, training
and retaining aged care workers.
-
Chapter 4 examines the increasing diversity of aged care
users, and the associated challenges in regional and remote community service
delivery, and the challenges faced by organisations in delivering a culturally
competent service both in regional and urban locations.
-
Chapter 5 concludes the committee's consideration and
makes recommendations for further consideration.
The changing aged care sector
1.7
The aged care sector is undergoing significant changes. The Australian
population is ageing, and at the same time the aged care user cohort is
becoming more diverse, with greater disparity in health status, disability,
location, cultural and language needs, sexual orientation and gender
identification. These changes are placing increasing pressure on the workforce
not only to meet the overall increased numbers of aged care recipients, but to
have the specialised skills needed to meet the increasing diversity of service
needs. This following section will outline the key changes occurring in the aged
care sector by overall population, and the diversity of specialised service
needs.
Increasing aged care service users
1.8
As at 30 June 2016, 15 per cent of Australia's population was aged 65
years and over (3.7 million people) and 2 per cent were aged 85 years and over
(488,000 people). By 2026, it is estimated that 18 per cent of the population
will be aged 65 years and over (5.0 million people) and 2.3 per cent (644,000
people) will be 85 years and over.[1]
1.9
By 2055, the proportion of Australians over 65 will increase to 22.9 per
cent (8.9 million) of the total population.[2]
The number of Australians receiving aged care is projected to increase by
around 150 per cent over the next 40 years.[3]
1.10
In 2009-10, around 616 000 people aged 70 years or older received home
and community care services (HACC).[4]
1.11
Between 1999 and 2011, the number of people moving into residential aged
care in Australia increased by 25 per cent, with the largest growing group
being those over 85 years of age. In 2014, 82 per cent of permanent aged care
residents required high-level care.[5]
1.12
Department of Health data shows that in 2015-16:
-
Over 1.3 million older people received some form of aged care:
- More than 640,000 older people received home support through the
Commonwealth Home Support Programme (CHSP);
- 85,432 older people received support through the
Commonwealth-State HACC program (Victoria and WA);
- 56,852 people received residential respite care;
- 88,875 people received care through a home care package;
- 234,931 people received permanent residential aged care.
-
the average age on entry for new admissions to permanent
residential aged care was 82.0 years for men and 84.5 years for women; and
-
around 50 per cent of all residential aged care residents had a
diagnosis of dementia.[6]
Aged care in rural and remote
communities
1.13
The committee notes that there are particular challenges for the
delivery of aged care in rural and remote areas. Thirty one per cent of older
Australians live in inner and outer regional areas, and approximately 1.5 per
cent of all Australians aged 65 years or older live in remote or very remote
areas.[7]
1.14
The proportion of older Australians in aged care in rural and remote
areas varies across the states and territories. In 2013–14, 30 per cent of
people in permanent residential aged care were located in rural or remote
areas: fewer than one per cent (0.7 per cent) in remote or very remote areas
and 30 per cent in inner and outer regional areas.[8] In New South Wales,
Victoria, South Australia and Western Australia, fewer than 30 per cent of permanent
aged care residents were in facilities in rural or remote areas; in Queensland
the proportion was 35 per cent.[9]
In the Northern Territory and Tasmania, all people in permanent residential
aged care were located in areas categorised by the Australian Bureau of
Statistics as regional or remote areas.[10]
1.15
In remote and very remote areas, aged care service provision may be
delivered by a very limited number of organisations, and in some cases by just
one provider. Local government is a key aged care service provider in remote
and very remote locations. For example, the MacDonnell Regional Council is the
only provider of disability and aged care services in eight remote Aboriginal
and Torres Strait Islander communities in Central Australia.[11]
1.16
The Australian Institute of Health and Welfare (AIHW) has noted:
People who live in rural or remote areas face additional
difficulties in accessing health and ageing related services. Rural and remote
areas have fewer services available, particularly in close proximity to where
people live, and the services that do exist may not be attainable, for example,
due to cost or lack of transport. In addition, service providers in rural or
remote areas face challenges in service provision: the costs of building and
operating facilities are higher, and there are fewer skilled workers available.[12]
Aboriginal and Torres Strait
Islander peoples in aged care
1.17
Aged care service delivery to Aboriginal and Torres Strait Islander
peoples has differing challenges from mainstream service delivery, not only
based on the need to deliver a culturally competent service, but also because
the demographics, health profiles and locations of these service users differ
significantly from the non-Indigenous population.
1.18
In 2014-15, 34 283 Aboriginal and Torres Strait Islander people accessed
residential aged care (2 279), Home Care (2 214) and Home and Community Care
(29 552), and 800 people accessed services through the Aboriginal and Torres
Strait Islander Flexible Aged Care program. In 2015-16, Aboriginal and Torres
Strait Islander peoples accessed the majority of residential places and home
care packages in remote and very remote locations.[13]
1.19
The committee notes that the age distribution of Aboriginal and Torres
Strait Islander peoples in aged care differs from the non‑Indigenous
population, with a younger age structure and shorter life expectancy. The
average life expectancy of the general population is about 73 years for women
and 69 years for men. Due to generally poorer health, conditions associated
with ageing may affect Aboriginal and Torres Strait Islander peoples earlier
than non‑Indigenous people. Owing to these factors, aged care planning
includes the Aboriginal and Torres Strait Islander population aged 50 and over,
rather than 70 and over as with the non-Indigenous population.
1.20
In general, the age profile of Aboriginal and Torres Strait Islander
peoples in residential facilities was substantially younger than that of
non-Indigenous people (Figure 1.1).
Figure 1.1: People in residential aged care, by age group
as a proportion of population by Indigenous status, at 30 June 2014.
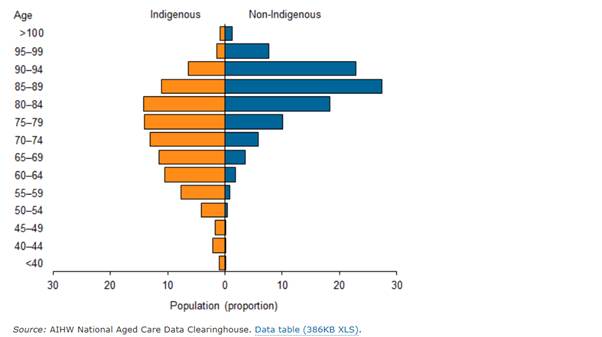
Source: Australian Institute of Health and Welfare, Indigenous
people in aged care webpage, (accessed 23 December 2015).
1.21
In all groups aged under 85 years, Aboriginal and Torres Strait Islander
peoples used residential aged care at higher rates than non-Indigenous people
of the same age (Table 1.1).
Table 1.1: Age and sex specific usage rates for people in
residential aged care by Indigenous status, at 30 June 2014 (per 1,000
population)
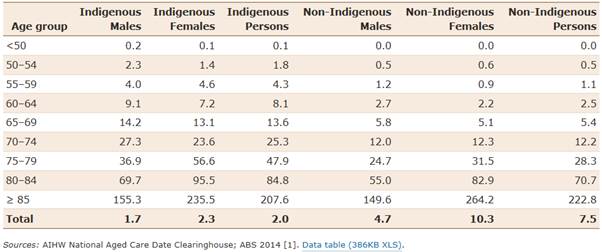
Source: Australian Institute of Health and Welfare, Indigenous
people in aged care webpage, (accessed 23 December 2015).
1.22
A higher proportion of Aboriginal and Torres Strait Islander aged care
residents are located in remote or very remote facilities across Australia than
non-Indigenous aged care residents. In New South Wales and Victoria, however,
where there are no aged care facilities in remote or very remote areas, all
aged care residents are in urban or regional aged care facilities. [14]
Culturally and linguistically
diverse (CALD) community in aged care
1.23
A key diversity challenge for the aged care sector is service delivery
to CALD communities. As outlined below, the proportion of older Australians
from CALD backgrounds is increasing, and, like Aboriginal and Torres Strait
Islander peoples, they utilise aged care services differently to
Australian-born aged care service users.
1.24
In 2011, 36 per cent of older Australians were born overseas, with 22
per cent from 'non-main English speaking countries'.[15] The older population of
Australia comes from a diverse range of countries, which is expected to
continue into the future (Table 1.2). The Australian Bureau of Statistics
examined the birthplace of the 0–64 age group in the 2011 Census and reported:
older Australians are more likely to be born in Australia, many as second
generation Australians the United Kingdom and Europe are becoming much less
dominant sources of immigrants, with strengthening proportions from India and
Sri Lanka, Lebanon, Vietnam, the Philippines, Malaysia, China, Hong Kong, South
Africa, New Zealand and other countries in the region.[16]
Table 1.2: Older persons born overseas, countries of
birth, 1981, 1991, 2001 and 2011(a)(b)
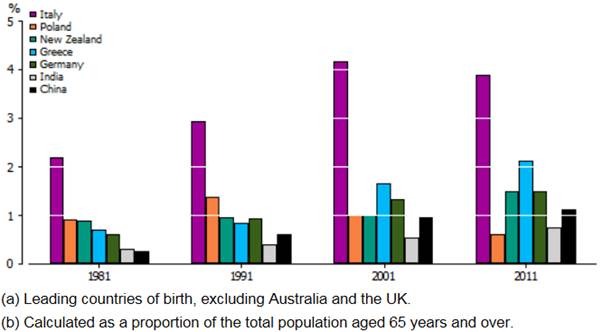
Source:
Australian Bureau of Statistics, Who are Australia's Older People?, Reflecting
a Nation: Stories from the 2011 Census, 2012, (accessed 22 December 2015).
1.25
The number of older Australians from CALD backgrounds is expected to
increase in future decades, in line with the overall increase in the older
population. In a 2001 study, the Australian Institute of Health and Welfare
forecast:
Between 2011 and 2026 the number of people aged 65 and over
from culturally and linguistically diverse backgrounds is projected to increase
from 653,800 to 939,800, a growth rate of 44% over the 15-year period. At the
same time, the number of Australian-born people aged 65 and over is projected
to increase by 59%. Older persons from culturally and linguistically diverse
backgrounds are projected to account for 22.5% of the older Australian
population at the beginning of the period, and 21.2% at the end.
Between 2011 and 2026 the proportion of the culturally and
linguistically diverse background population that is aged 80 and over is
projected to increase from 25.9% (compared with 27.5% for the Australian-born)
to 28.7% (compared with 22.4% for the Australian-born). The older population
from culturally and linguistically diverse backgrounds thus ends the projection
period with a considerably older population profile than the Australian-born,
having begun it with a considerably younger one.
The numbers for those aged 80 and over are projected to
increase from 169,500 to 269,600 (a 59% increase compared with 29% in the
Australian-born population). The proportion of people aged 80 and over who are
from culturally and linguistically diverse backgrounds is projected to change
from 21.8% to 25.2%. By 2026, then, one in every four people aged 80 and over
will be from culturally and linguistically diverse backgrounds.[17]
1.26
The cultural and linguistic diversity of older Australians is an
important consideration in the planning and delivery of appropriate aged care
services. Diversity may be reflected in a number of ways, such as:
-
attitudes to the elderly, expectations of family care giving,
roles of women and support groups, and beliefs about health and disability;
-
beliefs, practices, religions, behaviours and preferences which
can affect the propensity to use formal care services; and
-
English language proficiency, which can affect access to
information and services, communication of needs and participation in the wider
community.[18]
1.27
As a result, the use of aged care services by older Australians from
CALD backgrounds is different than that for many other older Australians, with
variation across programs, age groups and countries of birth (Table 1.3). In
general, people born in 'non-main English speaking countries' have higher usage
rates of non-residential care.[19]
Table 1.3: Use of selected aged care programs, by country
of birth(a) and age, 2010–11 (clients per 1,000 population)
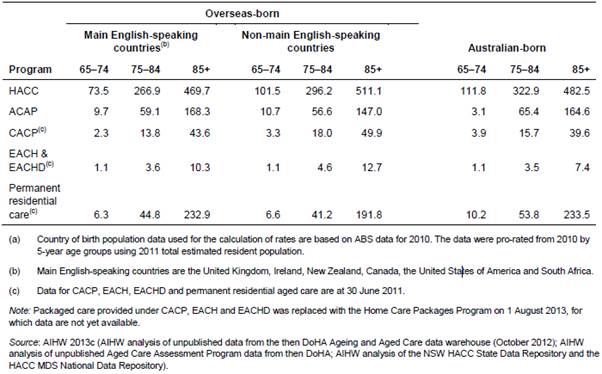
Source: Australian Institute of Health and Welfare, Cultural
and linguistic diversity measures in aged care, Working Paper, 2014, p. 8,
(accessed 22 December 2015).
1.28
Some CALD communities receive aged care services from providers, who
have tailored services to particular groups. However, the majority of older
Australians from CALD backgrounds access mainstream aged care services.[20]
Lesbian, Gay, Bisexual, Transgender
and Intersex (LGBTI) community in aged care
1.29
Many older LGBTI people have experienced discrimination over the course
of their lives on account of their sexual orientation and/or gender identity.
This discrimination can continue in aged care services, if older LGBTI Australians
are not recognised and supported in policy and practice.
1.30
At present, there is no data on the number and distribution of older
LGBTI Australians. However, it has been estimated that, in line with
Australia's growing ageing population, the number of older LGBTI Australians
aged 65 years and over is expected to reach 500 000 people by 2051.[21]
1.31
The 2016 Aged Care Workforce Survey found that:
-
11 per cent of residential aged care facilities cater for LGBTI
residents; and
-
of the 25 per cent of residential aged care facilities that cater
for a specific ethnic or cultural group, 44 per cent cater for LGBTI residents.[22]
1.32
There has been a significant increase in the proportion of home care and
home support service providers providing specialised services who now also cater
for LGBTI clients: in 2012, just one per cent of this group catered for LGBTI
clients; in 2016, this had risen to almost 41 per cent.[23]
Current composition of the aged care workforce
1.33
Just as the ageing population has changed in size and diversity, the demographics
of the workforce have also been shifting.
1.34
The aged care workforce consists of a variety of employment types,
including:
-
paid direct care workers, including personal care workers and
health care professionals;
-
paid non-direct care workers, including managers and ancillary
staff;
-
agency, brokered or self-employed staff; and
-
unpaid volunteers and informal carers.[24]
1.35
Latest research shows that the aged care workforce is predominately
female, has a higher than average median age, is largely employed on a
permanent part-time basis, and is disproportionality represented by Personal
Care Attendants (PCAs).[25]
1.36
The main source of data on the aged care workforce is the National Aged
Care Workforce Census and Survey (NACWCS), conducted by the National Institute
of Labour Studies (NILS) at Flinders University, on behalf of the Australian
Department of Health. The NACWCS is conducted every four years and collects
comprehensive data on the profile of, and identifies prevailing trends in, the
aged care workforce.[26]
The Aged Care Workforce, 2016, published in March 2017, contains the
most recent information and data.[27]
Direct care workers
1.37
In 2016, there were an estimated 235 764 workers in residential
care and 130 263 workers in home care and home support.[28]
The majority of these workers were employed in direct care roles.[29]
Figure 1.2: Direct care workforce, residential and
community care, by occupational group, 2016
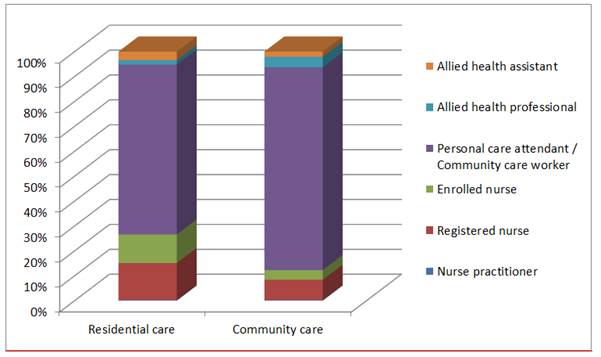
Source: National Institute of Labour Studies, Flinders
University, The Aged Care Workforce, 2016, Department of Health, Table 3.2,
Table 5.2.
1.38
Figure 1.2 shows that personal care attendants (PCAs)/community care
workers (CCWs) are the largest occupational group in the home care and home
support sector, representing nearly 84 per cent of workers.
1.39
Figure 1.2 also shows that, in 2016, PCAs constituted the majority of
the residential direct care workforce, whereas Registered Nurses (RNs) and
Enrolled Nurses (ENs) constituted a comparatively small proportion. Since 2012,
PCAs working in aged care have continued to increase both numerically and
proportionally. In contrast, the proportion of nurses in residential aged care
has declined.
1.40
Several submitters expressed concern that the number of qualified staff,
particularly nurses, working in aged care is declining.[30]
However, latest research appears to show that while the proportion of qualified
nursing staff in residential direct care roles has remained relatively steady,
their numbers (with the exception of ENs) have increased since 2012.[31]
The same trends have not been observed in the home care and home support sector
however, with latest data showing that qualified nursing staff has declined
numerically and proportionally since 2012.[32]
Volunteers
1.41
Volunteers are significant contributors to the aged care workforce, with
83 per cent of residential facilities and 51 per cent of home care and home
support outlets utilising volunteer staff. Several submitters argued that
volunteers have a crucial role in the workforce, and that future challenges cannot
be faced without their continued and increasing support.[33]
The role, services provided by, and future challenges impacting volunteers is
discussed in greater detail in chapter 2.
Allied Health Professionals
1.42
Allied Health Professionals (AHPs) represent a comparatively small
proportion of the workforce (particularly in residential care).[34]
Some submitters argued that AHPs are currently being underutilised, but will
increasingly be required to meet the complex needs of older people in care.[35]
The role of AHPs in helping to meet future workforce demands is discussed
further in chapter 2.
Characteristics of the aged care
workforce
1.43
The average aged care worker is likely to be:
-
female (88 per cent);
-
older (49 years old); and
-
located in a major city (around 2/3 of all workers).
1.44
Females represent the highest proportion of workers, accounting for 87 per
cent in the residential care sector, and 89 per cent in the home care
and home support sector in 2016. However, the proportion of males in the residential
aged care workforce has grown from 7 per cent in 2007 to 13 per cent in 2016. The
proportion of males in the home care and home support sector has not changed
significantly since the collection of data began in 2007.[36]
1.45
The latest iteration of the NACWCS found that the median age of the
residential direct care age workforce has decreased from 48 years in 2012 to 46
years in 2016. However, the median age of home care and home support workers
continues to grow, increasing from 50 years in 2012, to 52 years in 2016. Similar
trends have also been observed for recently hired employees in both sectors.[37]
1.46
Consistent with evidence received by the committee, the majority of the
workforce is located in major cities, with about one third located in regional
areas.[38]
1.47
A substantial proportion of aged care workers are overseas-born.
However, the overall proportion of the workforce born overseas has reduced
since 2012 to 32 per cent and 23 per cent in residential and home care
respectively. Despite this latest trend, the proportion of recently hired
employees in the residential sector that are overseas-born has continued to
increase.[39]
1.48
By comparison, Aboriginal and Torres Strait Islander people account for
a very small proportion of the workforce, representing around one to two per
cent of the total workforce.[40]
The role of governments in aged care
1.49
The Australian Government's role in the provision of aged care services
in Australia is in setting the regulatory framework and providing the majority
of funding to support aged care providers.[41]
1.50
At the federal level, aged care is administered by the department and
governed by the Aged Care Act 1997 and associated Aged Care
Principles.[42]
Aged care services in Australia are delivered by a range of not-for-profit
(religious, charitable, and community) and for-profit organisations, and
state/local government providers. The department provides funding to a large
number of these providers through various funding packages.[43]
1.51
The main programs funded by the department in the residential and
community based care sector include:
-
Residential aged care:
-
Permanent care: ongoing care in a residential aged care facility.
-
Respite care: temporary short-term care in a residential aged
care facility.
-
Community based care:
-
Commonwealth Home Support Program (CHSP): entry-level home-based
support services.
-
Home Care Packages Programme: for more complex, coordinated and
personalised home-based care.[44]
1.52
Australian Government funding represents the highest proportion of
revenue for aged care providers. In 2014-15, the Australian Government spent
15.2 billion on aged care.[45]
In 2015-16, Australian Government expenditure on aged care was $16.2 billion,
of which $11.4 billion was for residential aged care.[46]
1.53
The majority of aged care providers across all types of care are
not-for-profit organisations, with smaller proportions delivered by for-profit
and state, territory and local governments.[47]
1.54
In its 2017-18 Budget the Government announced that it will extend
funding arrangements for the CHSP and Regional Assessment Services for a further
two years.[48]
More recently, the Government announced increased funding of $649 million
per year to provide an additional 9911 new aged care places in the 2016-17 Aged
Care Approvals Round, with 2719 places reserved for services outside
metropolitan areas. Of the total places being made available 75% are reserved
for the development of new aged care services, including existing service
providers establishing new dementia specific units. An additional $64 million
funding for capital grants is available to assist organisations establish new,
or upgrade existing, facilities required to deliver their new aged care
services.[49]
Role of State and Territory
governments
1.55
Under the 2011 Council of Australian Government's (COAG) National
Health Reform Agreement, the Australian Government agreed to assume 'full
funding, policy, management and delivery responsibility' for aged care
services.[50]
Separate agreements were negotiated with Victoria and Western Australia, where
some home support services continue to be funded under the joint
state/Commonwealth Home and Community Care (HACC) program, with plans to
transition to the Commonwealth program at a later date.[51]
1.56
However despite the transition to full Commonwealth funding, it is clear
from evidence received by the committee that state and territory governments
continue to play an important role in the funding and delivery of aged care
services.[52]
1.57
For example, Queensland Health submitted that it provides 'about five
per cent of residential aged care places, the majority of flexible community
and residential aged care places...and a limited number of Home Care Packages and
Commonwealth Home Support program services'.[53]
Role of local government
1.58
The committee received evidence that local governments play an important
role in the delivery of aged care services, particularly in regional and remote
areas.
1.59
The Local Government Association of the Northern Territory (LGANT)
submitted that aged care services in remote Indigenous communities in the
Northern Territory (NT) are provided under contract by a number of regional
councils, which are 'cost sensitive' and rely on flexible funding arrangements
to support their workforce.[54]
LGANT noted that 'regional councils are well placed to provide a long term and
accountable option for the delivery of Commonwealth programs and currently do
so...'[55]
At the committee's hearing in Darwin, LGANT suggested that regional councils,
rather than for-profit providers are better placed to deliver aged care
services in remote areas of the NT, as it is not generally viable for
for-profit providers to deliver such services.[56]
1.60
In Victoria, local government also has an important role as the main
provider of community care through the HACC program.[57] Some Victorian local
government agencies suggested that greater funding will be needed to assist
with the transition of the HACC program to the Commonwealth from 2019.[58]
Australian Government funded aged care workforce measures
1.61
This section examines the role government currently plays in funding and
developing aged care workforce measures, and the role it should have in
developing any future national strategy.
1.62
The Australian Government funds a range of measures to support the aged
care workforce.[59]
1.63
In 2015, the Australian Government commissioned the Stocktake and
analysis of Commonwealth funded aged care workforce activities, which
examined 54 workforce specific activities that received funding between 2011-12
and 2013-14. The stocktake found:
-
the majority of Commonwealth funding was directed toward workforce
training, education and upskilling;
-
consideration should be given to supporting workforce planning
strategies, leadership development, regional and remote services, carers and
volunteers; and
-
program effectiveness needs to be better designed, measured,
demonstrated and shared through evaluation with input from the aged care
sector.[60]
1.64
Some submitters expressed concerns about recent changes to the funding
and structure measures for aged care, particularly the Aged Care Workforce Fund
(ACWF).[61]
1.65
The ACWF was introduced in 2011 to provide a flexible funding pool for
initiatives aimed at improving the quality of aged care, by developing the
skills of the aged care workforce. The ACWF:
-
provides access to training, education and other supports (such
as scholarships for nurses and financial support for aged care providers to
provide training places); and
-
provides targeted training and development strategies for
priority groups, including for Aboriginal and Torres Strait Islander peoples.
1.66
In 2015, the government announced that the ACWF would be combined with
the Rural Health Outreach Fund and the Health Workforce Fund into a single
Health Workforce Programme.
1.67
The department submitted that:
The merging of funds will enable the Government to develop
and drive workforce change across the health and aged care sectors that will in
turn benefit ageing Australians.
As part of the integration, Government support for aged
care-specific workforce activities will be integrated into health workforce
programs already available. In line with the Government's high prioritisation
of Indigenous employment issues, it will continue to provide significant
support and funding for workforce activities to provide access to health and
aged care services for Australians in hard to reach areas, such as for
Indigenous communities and in rural and remote areas.[62]
1.68
The Aged Care Financing Authority (ACFA) noted that this change
'reflected an overall reduction in funding for these programmes across the
forward estimates.'[63]
1.69
The committee received evidence from a wide range of groups across the
sector, including local government, not-for-profit and for-profit aged care
providers, and nurses and nursing unions concerning these changes. Many of
these submitters expressed concerns about the reduction in funding for the
ACWF, submitting that the ACWF has enabled them to provide education and
training that they may not have been otherwise able to provide.[64]
1.70
For example, the Local Government Association of the Northern Territory
(LGANT) indicated that further reductions to the ACWF would have the following
implications for remote and very remote aged care services and their workers:
-
the ability to continue to provide services at a high level would
be compromised;
-
the ability to employ qualified staff would be further
compromised;
-
the ability for aged care clients to remain on country would be
reduced, placing further pressures on residential facilities in regional
centres; and
-
services within communities would be compromised and potentially
reduced, and clients' dependent on services which provide regular nutritious
meals, water and personal care would be impacted.[65]
1.71
Not-for-profit providers also expressed concerns regarding the
streamlining and reduction of funding for the ACWF, and its impact on:
-
ability of providers to support training for workers;[66]
-
development of palliative care and dementia care skills;[67]
-
support for workers in regional and remote areas.[68]
1.72
Not-for-profit providers also noted the cap on fringe benefits tax
exemptions and its impact on their ability to attract and retain workers.[69]
1.73
In contrast, for-profit providers' main concern was the removal of the
payroll tax subsidy and its impact on the ability of private providers to
compete with not-for-profit providers.[70]
1.74
Nurses and nursing unions expressed concern that the removal of the
high/low care distinction for residential facilities may result in providers
cutting RN staff.[71]
This change is expected to be particularly acute in NSW, where it is currently
legislated that all high care facilities must have a RN on site at all times.[72] This issue is
discussed further in chapter 3.
Role of the Australian government
in developing an aged care workforce strategy
1.75
During the inquiry the committee heard evidence that suggested the need
for a national aged care workforce strategy to plan for and respond to future
challenges facing the aged care sector.
1.76
The committee heard overwhelming support for a collaborative, strategic
and targeted approach to the funding and design of a national aged care
workforce strategy.
1.77
The committee received a vast array of evidence from groups across the
aged care sector including not-for-profit and for-profit aged care providers,
unions, nurses, medical professionals and allied health practitioners who
considered that the Australian Government should:
-
take responsibility and leadership for development of an aged
care workforce strategy;[73]
or
-
work in consultation with the aged care sector to 'co-design' a
strategy.[74]
1.78
The National Aged Care Alliance (NACA), a national peak body of those in
the aged care sector, were particularly supportive of a co-design approach to
the development of a strategy. NACA recommended that the Australian Government:
...work with stakeholders to co-design a definitive workforce
development strategy to ensure a sufficient future workforce to meet the
service needs of health, aged care, disability and community service sectors
(including in regional and remote areas). This strategy should work towards
greater coordination across the social services sectors and should focus on
recruitment, retention, education, development and remuneration to ensure the
workforce needs of each of the sectors are met.[75]
1.79
COTA Australia, the national peak organisation representing older
Australians, agreed with this approach, stating that a national strategy will
only be effective 'if there is ownership of the development process by all
stakeholders', noting:
It is not sufficient, as some in the sector have tended to
do, to lay the primary responsibility on the federal government.[76]
1.80
The Department of Health (department) views the Australian Government's
role in the development of a workforce strategy as more of a 'facilitator',
rather than a leader.[77]
The department explained that the Australian Government's position on a
national aged care workforce strategy is that it will support the sector in
developing a strategy, but that it is ultimately the sector's responsibility:
Aged care employers are responsible, like any other employer,
for assuring that their workforce needs are aligned with their business
strategy, as an essential component of organisational governance.[78]
1.81
In its submission, the department further commented that government will
assist the sector in the development of a strategy 'by providing funding for a
sector-run development process, including provision for consultation with all
relevant parties'.[79]
1.82
Consistent with these comments, the Government announced in its 2017-18
Budget that it will:
...provide $1.9 million over two years from 1 July 2017 to
establish and support an industry-led aged care workforce taskforce and
contribute to the development of an aged care workforce strategy, including for
regional and remote areas.[80]
1.83
The department has explained that the taskforce will explore:
...short, medium and longer term options to boost supply,
address demand and improve productivity for the aged care workforce.[81]
1.84
The department has also commented that the strategy 'will connect with
the National Disability Insurance Scheme (NDIS) Integrated Market, Sector and
Workforce Strategy', and that the taskforce will consult within the sector, but
'also engage with other sectors, including disability, education and
employment'.[82]
1.85
The Government has not committed any additional funding for an aged care
workforce strategy, but stated the measure will be funded 'from within the
existing resources of the Department of Health'.[83]
1.86
The funding forms part of a broader $33 million dollar 'Boosting the
Local Care Workforce' workforce initiative to:
...assist providers in rural, regional and outer suburban
areas to provide the workforce required to meet the expected growth in the
disability and aged care sectors arising from the introduction of the National
Disability Insurance Scheme and an ageing population...[84]
1.87
The department has stated that the initiative will create 'regional and
specialist coordinators to assist NDIS and aged care providers to grow their
businesses and employ more workers'.[85]
The measure will be funded from within the existing resources of the Department
of Health, and Department of Social Services, and is discussed in greater
detail in chapter 4.
Committee
view
1.88
The committee notes that all levels of government have an important role
in aged care administration and expenditure, and providing funding and support
to the sector.
1.89
The committee considers that federal, state and territory, and local
governments have a role in assisting the sector to develop a national aged care
workforce strategy.
1.90
The committee is pleased that the Government has announced a commitment
to provide funding to assist to establish an industry-led aged care workforce
strategy.
1.91
The committee notes it will be important to ensure that stakeholder
consultation and engagement is properly organised to enable wide and meaningful
input from those who may be affected by any changes included in a national
workforce strategy.
Conduct of the inquiry
1.92
This inquiry was first referred by the Senate of the 44th
Parliament for inquiry on 1 December 2015, with a reporting date of 30 June
2016. The inquiry lapsed at the dissolution of the Senate on 9 May 2016.
1.93
On 13 September 2016, the Senate of the 45th Parliament agreed
to re-adopt the inquiry with a reporting date of 28 April 2017. On 20 March
2017, the Senate granted an extension of time for reporting until 21 June 2017.
Handling of submissions
1.94
During the first referral of this inquiry under the 44th
Parliament, a total of 296 submissions were received, 98 from organisations and
198 personal accounts from individuals, showing the depth of concern with this
issue from the general public.
1.95
In the second referral under the 45th Parliament, the
committee resolved not to call for new submissions but to rely on submissions
received during the 44th Parliament. All correspondence and evidence previously
received for this inquiry has been made available to the new committee. An
additional 13 submissions were received and accepted by the committee.
Public hearings
1.96
A total of 12 public hearings were held:
| 28 April 2016 |
Melbourne, VIC |
| 27 September 2016 |
Perth, WA |
| 28 September 2016 |
Bunbury, WA |
| 25 October 2016 |
Darwin, NT |
| 26 October 2016 |
Alice Springs, NT |
| 31 October 2016 |
Launceston, TAS |
| 3 November 2016 |
Canberra, ACT |
| 23 February 2016 |
Townsville, QLD |
| 6 March 2016 |
Wollongong, NSW |
| 7 March 2017 |
Adelaide, SA |
| 9 June 2017 |
Broome, WA |
| 13 June 2017 |
Canberra, ACT |
Navigation: Previous Page | Contents | Next Page