Chapter 3 - The nature and extent of illness and disability
3.1
The Committee was informed that the true nature and
extent of illness, disability and death due to toxic dust was difficult to
ascertain. Data sources rely primarily on workers' compensation data which is
limited in scope. While workers in some industries particularly the mining
industry are monitored regularly, this is not the case for all industries. The Construction,
Forestry, Mining and Energy Union (CFMEU) commented that the transient nature of
the construction industry, coupled with the possible delay in developing
symptoms, is an impediment to the accurate compilation of statistics. Many
workers move on to other industries and in some cases lung disease is attributed
to other causes for example, smoking.[60]
Data sources
3.2
Under the National Occupational Health and Safety Data
Action Plan, the National Occupational Health and Safety Commission (NOHSC) maintain
national occupational health and safety data. The primary data source used in Australia
is the National Dataset for Compensation-based Statistics (NDS) which consists
of accepted workers' compensation claims. Datasets are also maintained on
notified work-related fatalities and voluntary notifications of mesothelioma
cases. Other data sources include the National Hospital Morbidity data, the
National Coronial Information System, national surveys of households run by the
Australian Bureau of Statistics and surveys of GPs.
3.3
The Department of Employment and Workplace Relations (DEWR)
noted that a review of available data sources shows that there is limited
information on the extent of work-related respiratory disease in Australia.
Estimations of occupational contribution to respiratory disease in society are
difficult because respiratory disease can be attributable to other
non-occupational factors, unless it is specifically related to a unique
workplace causative factor or it can be differentiated by its clinical
features. The information that is available comes from a variety of sources,
including published studies; workers' compensation claims data, the Dust
Diseases Board (DDB) of NSW and the two Surveillance of Australian Workplace-Based
Respiratory Events (SABRE) programs in Victoria
and NSW. Published general practitioner and hospital presentation data sources
do not provide useable information, because respiratory disease cases are
included in categories that also contain such diseases not related to work.[61]
3.4
The Dust Diseases Board of NSW maintains statistical
information gathered from and about individuals who have attended a medical
screening or who have applied for compensation. Information includes:
-
new certificates of disablement issued
categorised by dust disease;
-
deaths categorised by causation and average age;
-
statistics relating to mesothelioma; and
-
medical data on individuals such as x-rays, lung
function tests etc.[62]
3.5
The SABRE project is a voluntary, anonymous
notification scheme of occupational lung diseases. It has been operating in Tasmania
and Victoria since 1997 and NSW
since 2001. It is supported by the Dust Diseases Board of NSW and is being
undertaken in collaboration with the team in London
who developed the Surveillance of Work-related Occupational Respiratory Disease
(SWORD) scheme. It also has links with New
Zealand. The aim of the SABRE project is to
determine the incidence of work-related respiratory disease and inhalation
injury in NSW and Victoria and to disseminate
information about the burden of occupational respiratory disease.[63]
3.6
Other witnesses commented on the lack of comparability
of datasets and the reliance on workers' compensation data. The Australian New
Zealand Society for Respiratory Science (ANZSRS) commented that the need for
consistency of approach in collecting data is becoming increasingly important
as the workforce becomes more mobile. Comparability of data would be in the
interest of gaining long term trending and separating pre-existing trends from
current trends.[64] WorkSafe Western Australia
informed the Committee that it recognised the difficulties associated with
collecting reliable data associated with toxic dust exposure, and it is working
with NOHSC to improve the availability and quality of data according to the NOHS
Data Action Plan.[65]
3.7
Workplace Health and Safety Queensland (WHS) commented
that, in undertaking research for its submission to the inquiry, it had found
it difficult to access data as there was a 'paucity of information of
significance held in a readily accessible form by any organisation, including
the State regulator' in all but the mining industry:
...there have been no identifiable programs for routine
collection of exposure data of the kind which will bring great substance to
these discussions...Industry, probably for reasons related to competition, has
not been motivated or sufficiently organised to fund and set up any scheme for
either data collection or shared data management. This situation applies not
only to those in dusty industries, but to almost all fields where exposure
occurs to hazardous substances with both short and long term health
consequences, but particularly long term exposures with chronic diseases. Only
in mining has there been a long standing arrangement of routinely collecting
dust exposure data by government bodies.[66]
3.8
WHS went on to state that only government seems to be in
a position to command the collection and analysis of data, however:
Efforts to establish such collections of data in Australia
on a national basis through either the National Institute for Occupational
Health and Safety or the NOHSC have come to nought, because of their lack of
continuity. Impartiality and independence in the national arena are now new
considerations. In the case of exposures to respirable crystalline silica, the
time frame must be many decades long. The Health and Safety Executive in the UK
has operated a mechanism into which such critical data from across the nation
can be collected and analysed.[67]
3.9
The Minerals Council of Australia (MCA) also noted that
workers' compensation data lacked detail and timeliness. In addition, a worker
needs to be off work for five days to be included in the workers' compensation
data, whereas the minerals industry records one day off in its statistics. MCA commented
that there is no central database to facilitate analysis, to establish trends
or to track the health of workers as they move from one company to another, or
to track any disease through their life. The data that are available are often
not available in electronic form, so analysis is not easy:
We believe that the focus has been very much on collection
rather than on analysis. In some organisations that do collect data, such as
government agencies, there are cupboards full of material but no resources to
analyse it.[68]
3.10
MCA also referred to the difficulties of tracking the
health of workers and commented that HealthConnect could be a useful means of
monitoring the health of workers in certain industries. HealthConnect collects,
stores, and exchanges health information under strict privacy safeguards. With
amendments to include information on occupation, MCA suggested that tracking
people after they had left the industry could be possible.[69]
3.11
The Australia Institute of Occupational Hygienists (AIOH)
pointed to the Health Watch study of workers in the Australian oil industry. This
is an independent epidemiology program which commenced in 1980. The program
studies the health of about 18,000 past and present employees in the petroleum
(oil and gas) industry. The Health Watch study could be adapted as a model to
study the incidence of occupational disease as a consequence of exposure to
toxic dusts in the workplace (such as exposure to silica in sandblasters).
However, AIOH also commented that the oil industry in Australia is made up of
just a few large, well-resourced companies and an active industry association that
are both able to draw upon occupational hygienists, occupational physicians and
epidemiologists. Most Australians, however, are employed in small to medium
sized enterprises, which do not have access to these levels of resources and as
a consequence, it is difficult to characterise the precise incidence and
prevalence of dust related disease in the general working population.[70]
3.12
Mr Bruce
Ham commented that work had been undertaken
to examine the possibility of a National Mining Health Database. The study
concluded that the current large mining health databases were very similar in
structure and had potential to be combined, especially for research purposes.
However, the existing legislative structures made a central database unlikely. Mr
Ham noted that the research potential of
using existing databases was demonstrated in a joint New South Wales Heart
Disease risk project. A feature of this research was the matching of the
register of miners with the Deaths Index held by the Australian Institute of
Health and Welfare. This has provided an important dataset for further health
outcomes research.[71]
3.13
The Australian Council of Trade Unions (ACTU) and CFMEU
also highlighted the need for improved data sources. The ACTU recommended
improvements in data collection across the jurisdictions, including
establishing a national medical registry of dust diseases cases. The ACTU
commented that one possible means was to make SABRE compulsory rather than
relying on workers' compensation data:
We need to look at improving the data collection; compulsory
reporting by the states, the jurisdictions, to this scheme; and perhaps
expanding it to the hospitals and GPs and other groups that deal on a daily
basis with people who have contracted airborne diseases. Until that happens we
do not get the right figures and therefore we do not know how big this problem
is and we cannot work out a good strategy, so that is essential.[72]
3.14
The Dust Diseases Board noted that:
The SABRE Scheme plays an important role in determining which
occupations and industries are likely to cause disease and why. Once known,
positive strategies can be developed to prevent lung diseases in these
industries and occupations. The Scheme has the potential to decrease the
incidence of occupational lung disease and to be of significant public health
benefit.[73]
Incidence of disease related to toxic dust
3.15
WHS stated that during the last 100 years, exposure to
dust has resulted in dust diseases which, in Australia,
have claimed thousands of lives and caused some incapacity and suffering to
tens of thousands of others. During the same period, control of dust exposures
following increasingly stringent dust standards has, with the noted exception
of asbestos, reduced present and future incidence of dust disease to a tiny
fraction of that previously observed. WHS commented that the coal mining industry
best illustrates the success of regulation with the prevalence of coalworkers'
pneumoconiosis declining from as high as 27 per cent before World War II and
16 per cent in 1948 to virtually non-existent levels by the turn of the
21st century.[74]
3.16
DEWR provided the Committee with an overview of the estimates
of the incidence of respiratory disease in Australia.
Population based estimates in Australia
are used to indicate the magnitude of premature mortality induced by exposure
to hazardous substances in the workforce. The estimated age-adjusted mortality
rates (expressed in number of deaths per million per year) were estimated to be
5 and 2 for asthma, and 8 and 0 for dust diseases, respectively in men and in
women. However, these estimates only addressed mortality, not morbidity.[75]
3.17
Workers' compensation-based estimates of rates of
work-related respiratory disease are limited as the information published at a
national level only includes cases that result in five or more days off work. A
proportion of respiratory disease cases will not be formally diagnosed or will
occur in workers after they leave work, in which case the connection to work is
unlikely to be established and a workers' compensation claim is unlikely to be
made. Also, a sizeable minority of workers has been shown not to be represented
in Australian workers' compensation statistics.[76]
3.18
Figure 3.1 shows the numbers of cases of accepted
claims for occupational respiratory diseases in Australia
over the three year period of 2001-2003.
Figure 3.1. Occupational
Respiratory Disease claims, Australia,
2001-2003 (NOSI)
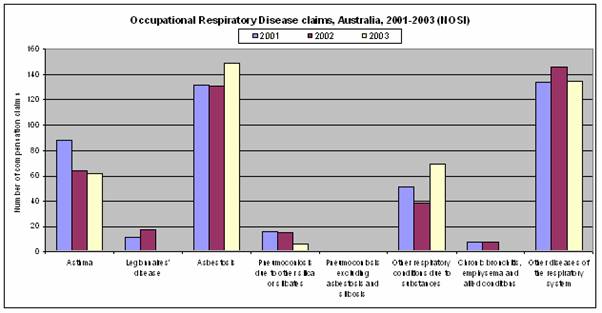
Source: Submission 11, p.6 (DEWR).
3.19
The most common occupational respiratory disease is asbestosis,
followed by asthma. Pneumoconiosis and chronic bronchitis are much less common.
Two of the more common categories are 'Other respiratory conditions due to
substances' and 'Other diseases of respiratory system'. DEWR also provided the
Committee with a breakdown of 'other respiratory conditions due to substances'
showing the number of accepted compensation claims against a causal chemical
agent. For example, industrial fumes and gases had 225 accepted claims from
1996-97 to 2003-04 while there were 635 claims for 'dust not elsewhere classified'.[77]
3.20
The three industries with higher disease claims are
manufacturing followed by education, and health and community services. In
manufacturing, asbestos related-disease is the main disease group (233 claims),
with asthma in the second group (59 claims). In education and health and
community services, claims are mainly in the 'Other diseases of the respiratory
system' group. When considering occupation groups, the higher number of claims
occur in professionals, associate professionals and labourers respectively.
Most claims occur in 'Other diseases of the respiratory system' for
professionals, while most claims for associate professionals and labourers are
asbestos-related disease.[78]
3.21
Table 3.1 shows the number of workers and dependents
who received compensation under the NSW dust diseases scheme during 2004-05.
Table 3.1: Compensation payments during 2004-05 by disease for the NSW
dust diseases scheme
|
Disease |
Workers |
Dependants |
TOTAL |
|
Asbestosis |
230 |
308 |
538 |
|
Silicosis |
188 |
276 |
464 |
|
Byssinosis |
2 |
7 |
9 |
|
Hard Metal
Pneumoconiosis |
3 |
2 |
5 |
|
Farmer's
Lung |
0 |
1 |
1 |
|
Aluminosis |
2 |
1 |
3 |
|
Bagassosis |
0 |
0 |
1 |
|
Asbestos
Related Pleural Disease (ARPD) |
449 |
112 |
561 |
|
Silico-Tuberculosis |
1 |
9 |
10 |
|
Asbestosis/ARPD |
63 |
23 |
86 |
|
Talcosis |
0 |
1 |
1 |
|
Silico-asbestosis |
4 |
2 |
6 |
|
Mesothelioma |
226 |
1244 |
1470 |
|
Lung
cancer associated with silicosis |
1 |
0 |
1 |
|
Silicosis/ARPD |
2 |
0 |
2 |
|
Carcinoma
of the Lung* |
20 |
85 |
105 |
|
Silica/Lung
cancer |
5 |
16 |
21 |
|
Silicosis/mixed dust
fibrosis |
0 |
1 |
1 |
|
Plueral plaques &
pain |
1 |
0 |
1 |
|
Mixed dust with
pneumoconiosis |
1 |
1 |
2 |
|
Lung cancer in
association with asbestos exposure |
12 |
100 |
112 |
|
Peritoneal mesothelioma |
16 |
46 |
62 |
|
TOTAL |
1226 |
2235 |
3461 |
* includes
Hexavalent chromium associated lung cancer, asbestosis/lung cancer & ARDP/lung
cancer
Source: Dust
Diseases Board of NSW, Making a
Difference Annual Report 2004/2005,
Appendix 5, p.70.
3.22
Table 3.2 shows data published by the Dust Diseases
Board of NSW on deaths by causation and average age since the inception of the Workers'
Compensation (Dust Diseases) Act on 29
February 1968.
Table 3.2: Deaths according to disease for the NSW dust diseases scheme
since 1968
|
Disease |
Death due to dust |
Death not due to dust |
Total |
Average age of death due to dust |
|
Asbestosis |
402 |
241 |
643 |
72.57 |
|
Silicosis |
435 |
944 |
1379 |
70.98 |
|
Byssinosis |
11 |
19 |
30 |
71.83 |
|
Hard Metal Pneumoconiosis |
2 |
3 |
5 |
63.43 |
|
Farmer's Lung |
1 |
2 |
3 |
61.17 |
|
Aluminosis |
0 |
1 |
1 |
- |
|
Bagassosis |
0 |
1 |
1 |
- |
|
ARPD |
168 |
89 |
257 |
75.70 |
|
Silico-Tuberculosis |
8 |
12 |
20 |
62.80 |
|
Asbestosis/ARPD |
32 |
25 |
57 |
76.83 |
|
Emery Pneumoconiosis |
0 |
1 |
1 |
- |
|
Talcosis |
1 |
2 |
3 |
65.74 |
|
Silico-asbestosis |
10 |
4 |
14 |
67.31 |
|
Mesothelimoa |
1812 |
8 |
1820 |
67.98 |
|
Peritoneal Mesothelimoa |
2 |
0 |
2 |
63.45 |
|
Carcinoma of the Lung* |
213 |
2 |
215 |
68.69 |
|
Silicosis/Lung Cancer |
25 |
0 |
25 |
71.41 |
|
Silicosis/Mixed Dust Fibrosis |
3 |
0 |
3 |
72.60 |
|
Mixed Dust Pneumoconiosis |
1 |
0 |
1 |
61.47 |
|
Lung Cancer in Association with
Asbestos Exposure |
109 |
4 |
113 |
68.35 |
|
TOTAL |
3235 |
1358 |
4593 |
68.37 |
*
includes Hexavalent Chromium Associated Lung Cancer, Asbestosis/Lung Cancer and
ARPD/Lung Cancer
Source: Dust
Diseases Board of NSW, Making a
Difference Annual Report 2004/2005,
Appendix 5, p.70.
3.23
The Dust Diseases Board also provides information on
the proportion of compensation payments made for asbestos and silica diseases
and all lung diseases. Figure 3.1 shows that asbestos-related compensation
accounted for 90 per cent of the compensation payments made by the Board from
1994 to 2005. Silicosis lung cancer accounted for 8 per cent of the dust
related lung cancers compensated by the Board in the same period.
Figure 3.1: NSW Dust Diseases
Board Compensation payments 1994-2005
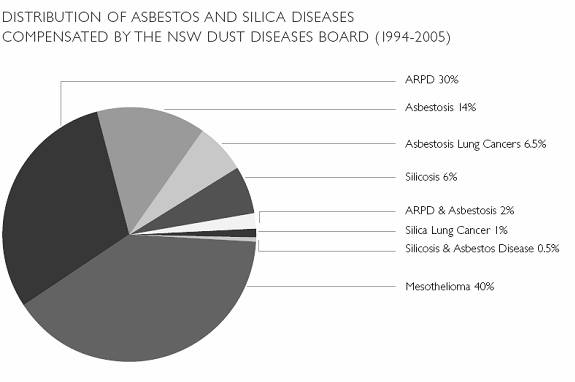
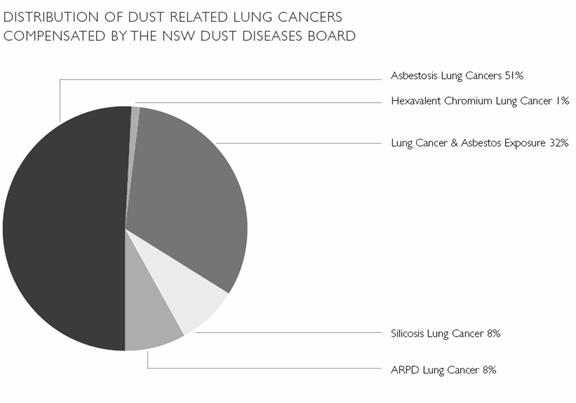
Source: Dust Diseases Board of NSW, A
Guide to Compensated Occupational Lung Disease in NSW, p.15.
3.24
Information from the Dust Diseases Board only shows
data for cases where compensation has been paid. Therefore, these figures do
not include other lung diseases or other diseases caused by occupational
exposure to dust, or unsuccessful cases for compensation.
3.25
A further source of data is the SABRE notification
scheme. For Victoria and Tasmania,
the most common condition reported by physicians is asthma (33 per cent of
occupation respiratory events reported). The asthma incidence rate is 30.9 per
million workers per year with a 2.4 times higher incidence rate in men compared
to women. However, DEWR noted that SABRE in Victoria
and NSW has incomplete coverage of physicians who see cases. The two most
commonly reported causative agents for asthma in the SABRE (Victoria)
notification scheme are wood dust and isocyanates (13.5 per cent and 5.8 per
cent respectively). The finding of asthma as the most commonly reported
occupational respiratory disease is similar to that found in overseas physician
notification schemes. The next most commonly reported condition in Victoria
and Tasmania is non-malignant
pleural disease from asbestos exposure.[79]
3.26
DEWR also provided rates compensation and
hospitalisation arising from inorganic dusts other than asbestos. For pneumoconioses
other than asbestos, there was a decrease in the hospitalisation rate. This may
be because the curves reflect different time periods in the history of the
disease; or there may be better treatment available, which means less
hospitalisation. In 2001-02 there were 72 hospitalisations, with 20
workers' compensation cases accepted. The hospitalisation numbers may include
the same individual presenting for multiple hospitalisation during the year. Workers'
compensation cases slightly increased, from 1.8 cases per million employed in
1998–1999 to 2.2 cases per million employed in 2001-02.[80]
3.27
While asbestos exposure in the workplace has decreased
over the last 40 years, asbestos related disease has a period of long
latency and it has been estimated that the incidence of asbestos related
disease will continue for the next ten to fifteen years. Data provided by DEWR
showed that asbestos-related workers' compensation cases increased from 10.1
cases per million employees in 1998-99 to 16.0 cases per million employees in
2001-02. Compensation cases for mesothelioma during the same period increased
from 5.4 cases per million to employees to 7.4 cases. Hospitalisations for
mesothelioma were higher.[81]
Incidence of disease related to
exposure to respirable crystalline silica
3.28
Submissions noted that health problems associated with
exposure to crystalline silica dust have been under investigation and control
in Australia
for more than a century. In 1905, investigation of the hard rock mining
industry in Western Australia was
carried out. In 1914 a Royal Commission was appointed to investigate safety
issues in Broken Hill mines. Surveillance by the NSW Silicosis Board (now the
Dust Diseases Board) and NSW Health Department resulted in the investigation
and control for Sydney
sandstone workers.[82] Regulations to
control dust disease were enacted in Western Australia
and New South Wales by the 1920s.
Dust disease was largely due to silica dust and tuberculosis.[83]
3.29
An exposure standard was set for silica in 1983-84 with
the National Health and Medical Research Council (NHMRC) recommending exposure
standards specifically for quartz (0.2 mg/m3), cristobalite (0.1 mg/m3) and
tridymite (0.1 mg/m3). In 1988 the exposure standard was reconsidered and a
reduction to 0.1 mg/m3 for respirable fraction of quartz, silica (fused) and tripoli
and 0.5 mg/m3 for cristobalite and tridymite was recommended. Following
public comment, it was agreed that further examination of the issue was
warranted. Between 1988 and 1996 no formal national exposure standard for
crystalline silica existed although some mining and OHS authorities issued
their own. From 1996, NOHSC reinstated the original NHMRC exposure standard. On
1
January 2005, a
revised national exposure standard of 0.1 mg/m3 for
quartz, cristobalite and tridymite came into effect.[84] (The new exposure standard is
discussed further in chapter 5).
3.30
While regulations were introduced to control silica
dust and appear to have had an impact on silica-related disease, NOHSC has
noted that 'due to a long lag time between exposure and symptoms, it is
difficult to ascertain how many people develop silica-related conditions, and
when the causative exposure occurred'. In addition health statistics do not
readily identify health problems related to exposure to RCS due to poor diagnosis
and lag times and, as noted above, compensation data relates only to cases for
which compensation has been paid.[85]
(Diagnosis of dust related health problems is discussed in chapter 4).
Silicosis
3.31
It was acknowledged in evidence that regulation has had
an impact on the exposure of workers to RCS, however, there was considerable
discussion on the incidence of silicosis in Australia
today and the incidence in particular industries. Some witnesses stated that
silicosis was now not a problem while other witnesses argued that silicosis was
'the new asbestosis'.
3.32
Witnesses pointed to a number of reviews and research
papers on the incidence of silicosis which indicated a decrease in the number
of cases of silicosis. In 1993, a review by the National Occupational Health
and Safety Commission of the state by state silicosis records indicated that
there were probably less than 20-30 new cases per year and the generality was that
these cases arose from uncontrolled exposure situations (that is, industries
and occupations where there was minimal or negligible adherence to the
legislative exposure standard and control requirements).[86]
3.33
Reviews of data on new cases of silicosis from the
mining industry have indicated that the incidence of silicosis has fallen. In Western
Australia, for example, there were only three cases
where the person had commenced employment after 1968 and none after 1994. It
was concluded that the absence of cases 'corresponds to the implantation of the
0.2 mg/m3 respirable
crystalline silica exposure standard in Western Australia...when the new cases
still arising as a legacy of the past have all been accounted for, new
incidences of this disease will have been virtually eradicated.'[87] Coal Services NSW also noted that for
the last decade there had been no incidence of silicosis that has been brought
to its attention. This reflected the safety management of companies and the
educational program that has been given to coalminers.[88]
3.34
AIOH also commented
that a review of the statistics commissioned by Worksafe Australia
in 2004 substantiated the small number of new cases of silicosis arising from
Australian industries.[89]
3.35
WHS also provided a review of known compensable cases
of silica related disease in Queensland.
Between 1992 and 2004 there were six claims for silicosis provided by the
Queensland Employee Injury Data Base. WHS stated that the evidence related to
incidence of compensable silicosis is rare and extremely limited for Queensland
workers as a whole and for abrasive blasting workers in particular.[90] It noted that some early exposures to
crystalline silica (prior to 1995) in sandblasting are likely to have been
excessive in modern day terms, though the compensation data do not reflect any
cases of silicosis.[91]
3.36
AIOH noted that silicosis numbers had declined. This
was due to a combination of regular medical surveillance, and reduction in
exposures such as compliance with a regulatory exposure standard, the
prohibition of specific tasks associated with high risk (such as sandblasting
and the use of silica flour in foundry operations) and the use of adequate dust
suppression systems such as ventilation and wetting down.[92] AIOH concluded:
Media headlines often imply that silica is "the new
asbestos". However examination of the data suggests otherwise. Silica has
been under surveillance for many decades, and the morbidity and mortality of
large populations of heavily exposed individuals have also been studied over
many decades. Clinical silicosis is now a rarity, and elevated risk of lung
cancer appears to be confined to cases where the silica exposure is of such a
level that it results in clinical silicosis. Based on the number (say 10-30) of
new cases of silicosis, this would amount to only 1 or 2 additional lung cancer
cases per year across Australia.[93]
3.37
The Cement Concrete and Aggregates Association (CCAA)
also stated that in the heavy construction materials industry 'even very early
or mild cases have been very rarely seen in this industry over the past 10
years. Those which have been diagnosed in that time all result from exposures
from at least 10 years ago.' CCAA concluded:
It is CCAA's view that in the heavy construction material
industries, substantial reduction of potential exposure has occurred, with
predicted and proven advances in dust control. In addition, the improved use of
personal respiratory protection has also reduced the risk of silicosis to
workers to its present extremely low level in Australia.[94]
3.38
Dr John Bisby remarked that in Australia in the last 50
years silicosis 'has been a fairly mild disease...But it can cause incapacity, so
it may reduce quality of life as opposed to reducing life expectancy, although
it can reduce life expectancy particularly in severe cases'.[95] Dr
Bisby, while conceding problems in certain
instances like sandblasting, also stated:
The silica issue is, in medical terms, basically over. It is a
great success story. Australian industry is free of silicosis, by and large.
That is not to say an occasional case may not happen, just like a truck
accident happens when somebody does the wrong thing. Basically it is
historical.[96]
3.39
Professor E
Haydn Walters
responded to this evidence and stated that:
I suppose it is true as far as it goes, I would say. In very
well regulated industries in which the conventional standards of dust exposure
are maintained, I would agree that interstitial lung problems, the traditional
pneumoconiosis, are now probably largely a historic issue. However, I think
those industries where the regulations are not vigorously upheld – and I think
a number of people have made rather off-the-cuff comments about cowboys in sandblasting
and that sort of stuff – still exist, and silicosis will still appear in time
because it is related to the amount in the atmosphere and the length of time
that you are exposed. If you are above the current threshold, then I think you
are still in danger of getting silicosis.[97]
3.40
In its Regulation Impact Statement, NOHSC sounded a
note of caution on the impact of the then exposure standard:
As diseases caused by exposure to RCS are of long latency,
current cases of adverse health effects could reflect the effect of past
exposures, when exposures were potentially greater than they are now under the
current standard. Therefore current cases may be an over-estimate of the effect
of the current NES [National Exposure Standard].
Conversely, the current NES...may be achieving their objectives,
which is why there are few incidents of adverse health effects recorded in
statistics. In addition, this could be a reflection of the under-reporting of
adverse health effects resulting from RCS exposure in official health
statistics.[98]
3.41
Other witnesses commented that silicosis is still a
significant disease. The CFMEU pointed to data from the Dust Diseases Board
which indicated that there were 200 cases each year and 'those are the ones
that are actually accurately diagnosed by the medical profession as having
silicosis'.[99]
3.42
Munich Holdings of Australasia provided the Committee
with a recent publication from the Munich Re Group on the impact of silicosis.
The paper noted that US insurers had been observing an increase in
silica-related claims. It was also noted that while claims were rising
strongly, the number of deaths from silicosis is declining steadily which
reflected the increased workplace safeguards from the 1970s on.[100]
3.43
Other researchers have also stated that 'it is
generally well known that the majority of workers exposed to crystalline silica
in Australia
work outside the mining industry'.[101]
The particular concerns of sandblasting were raised in evidence. WHS stated
that there was some evidence that during the period up to the late 1980s that
some silica exposures would have been occurring during abrasive blasting
operations which did not comply strictly with the regulatory requirements of
the time. WHS also commented that:
How much the silica dust exposure which did occur during the
1960s, 70s and 80s is likely to have contributed to silicosis cannot be fully
identified as reliable compensation statistics have been provided only as far
back as 1992. Given that the latency of silicosis will be around 20 to 30 years
(depending on years of first exposure and other factors), radiological
confirmed cases ought to have been appearing from 1990 through to the present.[102]
3.44
There are now various prohibitions in place relating to
free silica in abrasive blasting (NSW, WA, Tasmania); more than 5 per cent free
silica in abrasive blasting (SA, WA, Tasmania, NT) and more than one per cent
crystalline silica for abrasive blasting in Victoria and 2 per cent in Western Australia.[103] Mr
Nickolas Karakasch
noted that the United Kingdom
was one of the first countries to prohibit sandblasting. NSW prohibited sandblasting
in 1959, with the other States following some time later. Victoria
did not prohibit this activity until 2002.[104]
Blasting media that could be substituted include garnet, metal shot and
aluminium oxide.
3.45
Mr Karakasch
also stated that a 1987 report by the International Agency for Research into
Cancer (IARC) indicated that sandblasters in the USA
had the highest potential exposure to silica content of respirable dust. This
ranged from 4.8 – 12.2 per cent. Mr Karakasch
concluded:
Considering the sandblasting methods in Australia
and throughout the world were basically the same, it would not be unreasonable
to assume that sand blasters throughout Australia
were exposed to similar levels as reported in the 1987 USA
report. In comparison to the Victorian figure it is between 5 to 12 times the
allowable limit.[105]
3.46
AIOH also commented that the impact of the prohibition on
eliminating the use of silica/silica containing materials in sandblasting is
unknown. However they pointed to a 2001 report on the results of a blitz by the
Department of Workplace Health and Safety on abrasive blasting operations
throughout Queensland. This survey
found that of 49 operations audited, two (4%) were using dry sand. Other
than the two (4%) using sand, they also found that garnet was used as a
major blasting medium while others used ilmenite, different types of metal
refinery slags and metal shot. One operator used sodium bicarbonate. A small
number were using glass. WHS concluded that 'use of quartz bearing sands is now
low, but the 2 cases observed were found to contain silica between 58 – 78%
free silica. These operations were issued with Prohibition Notices.'[106] AIOH also commented that most
industries are now using substitutes such as garnet.[107]
3.47
AIOH provided details of a review of silicosis
sufferers who had received compensation in NSW. This showed that only just over
one per cent (less than one case per year) of people, who were receiving
compensation prior to 1970 and were still alive in 1970 and those who were
awarded compensation from 1970 to 1994, indicated that they did sandblasting as
part of their work. Most of these sandblasting cases were exposed around 1970
or earlier.[108]
3.48
CCAA commented on the unsatisfactory practices in some
industries and stated that 'the level of exposure that an unprotected
sandblaster might be exposed to is several hundred times the level of the
standards'.[109]
Airway disease
3.49
Professor Trevor
Williams concurred that there had been
'substantial reductions in classic silicosis'. However, he stated that 'it has
become apparent...that a new pattern of disease is emerging'.[110] People who have been exposed to
silica are now presenting with diseases including obstructive lung diseases and
pulmonary fibrosis. There is also propensity for dust such as silica to
increase the risk of the development of lung cancer and stomach cancer. He
commented:
I am also concerned that many patients with so called idiopathic
pulmonary fibrosis may have the genesis of their disease in exposure to fine
dust such as silica and that causal link is not made because of a long delay from
exposure to overt disease.
I don't believe we have sufficient information to even start to
understand the extent of these problems in Australia
and well designed studies are urgently needed.[111]
3.50
Professor Walters
also raised concerns about the incidence of COPD due to dust. He stated that the
contribution of dust, particularly in occupational settings, to subtler forms
of respiratory disease, and particularly to COPD, has been ignored. The
Professor also stated that as cigarette smoking becomes less, and also as more
vulnerable groups, particularly women, move into the workplace, the impact of
these dusts upon airway disease and the acceleration of the natural ageing
process of the lungs by exposure to dust is now becoming a significant feature,
and that is not being represented.[112]
3.51
The Professor informed the Committee that research data
are emerging that shows that these conditions of COPD related to dust,
particularly in the workplace, are perhaps more common than people have thought.
Research published in June 2005 in the journal Thorax by Professor Walters
and a research group in Victoria
found in a random survey of 4 000 or 5 000 people working and living
in the suburbs of Melbourne,
aged between 45 and 65, that there was about 10 per cent COPD in the
population. The Professor stated:
...particularly amongst the women, it was quite evident that
occupational exposure, particularly to biological substances but also to
mineral dust, was having an impact. It was a fairly subtle impact, but a
definite statistically significant impact upon their lung function. That
included people like nurses and those working in bakeries and so on who were
exposed to dust.[113]
3.52
However, AIOH commented that removing the smoking
component from airways disease and the reduced contemporary silica dust
exposures would mean only a few additional cases of airways disease per year in
Australia.[114]
Costs associated with adverse
health effects
3.53
NOHSC, in undertaking the review of the crystalline
silica exposure standard in 2004, provided costs associated with adverse health
effects. It was estimated , using NSW and national data, that the annual cost
of disease related to past exposure to crystalline silica in Australia
is in the order of:
-
$14,022,857 in compensation payments (including
medical costs, an indicator of potential cost) per annum;
-
305 hospital days per annum; and
-
60 lives per annum.[115]
NOHSC noted that health statistics used did not include
non-fatal conditions, such as disease or a restriction of function that does
not result in hospitalisation as these data are not available.[116]
Incidence of disease associated
with beryllium
3.54
Workers in Australia
have been exposed to beryllium dust. However, Mr
John Edwards
commented that the number who may have Chronic Beryllium Disease (CBD) is
unknown as until very recently there has been no dedicated Beryllium Blood
Lymphocyte Proliferation Testing (BeLPT) laboratory.[117] Workers most at risk are those in
the aviation industry as well as Navy personnel as a result of the descaling of
ship surfaces and workers in the alumina industry.[118]
3.55
In the United States,
the Department of Energy (DOE) is compensating DOE workers for exposure to
airborne beryllium. As at March 2006 DOE had approved 3034 beryllium claims and
paid out US$303.5 million in worker compensation in addition to $91 million in
medical costs. Mr Edwards
argued that the exposure of Australian workers to dusts, fumes and aerosols
containing beryllium materials is no different from the USA
so that cases are expected to be identified in Australia
with the establishment of a testing laboratory.[119]
Conclusions
3.56
Evidence received by the Committee points to a need to
improve the data available for identifying the incidence of disease related to
toxic dust. At the present time, there is a lack of comparability of datasets
and a reliance on workers' compensation data which may not indicate the true incidence
of toxic dust-related disease in Australia.
Workers' compensation data only includes those workers who have had five or
more days off work with a successful claim of a work-related illness. Where
diagnosis occurs after a worker has left work, the connection to work is
unlikely to be established and a workers' compensation claim is unlikely to be
made. This may lead to significant under representation of dust disease.
3.57
Witnesses called for a more comprehensive collection
system including the establishment of a national medical registry of dust
diseases cases. A national registry would assist in tracking workers as they
move from job to job. It would also provide more timely data to improve identification
of trends in disease. One possible means suggested to the Committee was to make
the SABRE system compulsory.
3.58
The Committee agrees that there is need to improve data
collection. Without reliable data, the true extent of dust-related disease is
unknown, trends cannot be identified in a timely manner and decision-making by
government, industry, unions and the medical profession is hampered.
Recommendation 1
3.59
That the Australian Safety and Compensation Council
review the National Data Action Plan to ensure that reliable data on disease
related to exposure to toxic dust is readily available.
Recommendation 2
3.60
That the Australian Safety and Compensation Council extend
the Surveillance of Australian Work-Based Respiratory Events (SABRE) program
Australia-wide and that the program provide for mandatory reporting of
occupational lung disease to improve the collection of data on dust-related
disease.
3.61
The incidence of toxic dust-related disease in Australia
today was debated extensively in evidence. Some witnesses commented that cases
of silicosis now emerging reflect past exposures and past work practices and
that silicosis is now a mild disease. However, other witnesses argued that
silicosis is the 'new asbestosis'. The Committee acknowledges that while the
data may under represent the incidence of disease, the available data suggests
that systems now in place to control dust related disease, particularly
silicosis, appear to have had a positive impact on the incidence of disease. Workers'
compensation cases of pneumoconioses other than asbestosis have increased only slightly
since 1998-99 from 1.8 cases per million to 2.2 cases per million in 2001-02.
3.62
However, the Committee notes that with apparently low
mortality from exposure to toxic dust, the economic cost of this level of
disease is still significant. NOHSC estimated in 2004 that compensation costs
for disease related to exposure to crystalline silica is in the order of $14
million per annum. The compensation costs for asbestos are substantially
higher. Compensation costs related to exposure to other dusts such as beryllium
are unknown but may be significant in the future.
Navigation: Previous Page | Contents | Next Page