Chapter 1 - Introduction
Terms of Reference
1.1
On 11 May 2006, the Senate, on the motion of Senators Moore, Allison and
Ferris, referred the following matters to the then Senate Community Affairs
References Committee for inquiry and report by 19 October 2006:
Gynaecological cancer in Australia
and in particular the:
- level of Commonwealth and other funding for research addressing
gynaecological cancers;
- extent, adequacy and funding for screening programs, treatment services,
and for wider health support programs for women with gynaecological cancers;
- capability of existing health and medical services to meet the needs of
Indigenous populations and other cultural backgrounds, and those living in
remote regions;
- extent to which the medical community needs to be educated on the risk
factors, symptoms and treatment of gynaecological cancers;
- extent to which women and the broader community require education of the
risk factors, symptoms and treatment of gynaecological cancers; and
- extent to which experience and expertise in gynaecological cancers is
appropriately represented on national health agencies, especially the recently
established Cancer Australia.
Conduct of the Inquiry
1.2
The inquiry was advertised in The Australian and through the
Internet. The Committee invited submissions from Commonwealth, State and
Territory Government departments and other interested organisations and
individuals. The Committee continued to accept submissions throughout the
inquiry.
1.3
The Committee received 72 public and 7 confidential submissions. A list
of individuals and organisations that made public submissions to the inquiry
together with other information authorised for publication is at Appendix 1.
1.4
The Committee held public hearings in Canberra, Sydney, Melbourne and Perth.
In organising its hearing program, the Committee endeavoured to hear from as
many individuals and organisations that represented and supported women with
gynaecological cancers. The Committee also heard from three witnesses from the United
States via teleconference and videoconference. A list of the witnesses who
gave evidence at the public hearings is available at Appendix 2.
1.5
The Committee was pleased to undertake interesting and valuable
inspections in Perth and Sydney. In Perth, the Committee had the opportunity to
visit the Menopause Symptoms after Cancer Clinic at King Edward Memorial Hospital.
In Sydney, the Committee visited the National Breast Cancer Centre and
discussed The Ovarian Cancer Program. The Committee also held private
discussions with Professor David Currow, CEO of Cancer Australia.
The Committee's report
1.6
Due to the broad range of issues covered within the Inquiry's terms of
reference, the Committee has grouped related themes and topics together and allocated
chapters accordingly.
1.7
Chapter 1 provides a general overview of the inquiry and provides information
to give a basic understanding of gynaecological cancers. Chapter 2 discusses
the concerns about the lack of attention given to gynaecological cancers at the
national level and contains the major recommendation proposing that separate
seed-funding be given to establish a national body focusing exclusively on
gynaecological cancers.
1.8
The remaining chapters present and discuss evidence received on the
terms of reference. Chapter 3 considers the appropriateness of current
levels of funding for research. Chapter 4 discusses the adequacy of
current screening, treatment and health support programs for women.
Chapters 5 and 6 consider the information needs of the medical community, women
and the broader community. Chapter 7 examines the extent to which gynaecological
cancer expertise and experience is represented in national agencies, including
Cancer Australia.
Background to the Inquiry
1.9
On 23 June 2005, the Senate tabled its report – The cancer
journey: informing choice.[1]
This inquiry considered matters relating to the delivery of services and
options for treatment of persons diagnosed with cancer and the role of less
conventional and complementary cancer therapies and medicines in treatment. The
Commonwealth Government tabled its response to this report on 22 June 2006.
1.10
Evidence received during the current inquiry into gynaecological cancer in
Australia raised concerns on the content of the Commonwealth Government's
response to the Senate Committee's recommendations. The Cancer Council of
Western Australia stated:
We are greatly disappointed about the lack of meaningful
response to and action on these recommendations. We are very hopeful that this
will not be the case in relation to any recommendations out of this [Gynaecological
Cancer in Australia] inquiry. We welcome this inquiry.[2]
1.11
The precursor to the current inquiry came on 7 December 2005, when
the Senate, on a motion of Senator Allison (on behalf of eight cross-party
Senators) referred a petition tabled on 6 December 2005 from 2,887
signatories on the management and prevention of gynaecological cancers and
Sexually Transmitted Infections (STIs) to the Committee for response to the
Senate by 30 March 2006. The Committee convened a Roundtable discussion on
3 March 2006 in Canberra, from which the Committee recommended that a detailed
inquiry into gynaecological cancers issues was warranted.
What are gynaecological cancers?
1.12
The term 'gynaecological cancers' refers to all cancers of the female
reproductive tract. The specialist doctors trained to treat these cancers are
gynaecological oncologists. A brief overview of gynaecological cancers is
provided below including a diagram, symptoms, incidence and survival
statistics.
Diagram 1: The Female Reproductive Organs
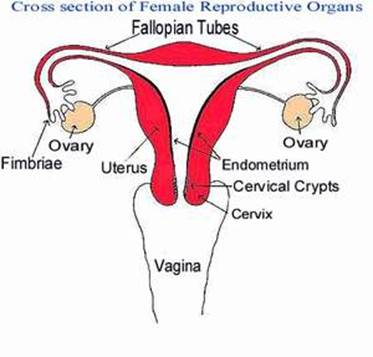
Source: www.menstruation.com.au/pubertyplace/changes.html
The types of gynaecological cancers
1.13
Gynaecological cancers comprise of cancers of the:
- ovary;
- fallopian tube;
- uterus;
- cervix;
- vagina;
- vulva; and
-
placenta and gestational trophoblastic disease (pregnancy related
cancers).
Risk factors for gynaecological cancers
1.14
Any woman is potentially at risk of developing a gynaecological cancer. While
the exact causes of gynaecological cancers are not known, some factors that may
play a role in the development of these cancers have been identified. These
include:
- age;
- smoking;
- family history of cancer;
- women whose mothers were given the hormone diethylstilbestrol
(DES) during their pregnancy;
- being overweight or obese; and
- personal history of cancer.
1.15
Also, certain subtypes of the human papilloma virus (HPV) have been identified
as a major risk factor in the development of cervical cancer.[3]
1.16
The risk factors vary according to the type of gynaecological cancer and
the occurrence of one or more of these risk factors do not necessarily mean a woman
will develop a gynaecological cancer.
Prevention of gynaecological cancers
1.17
As the causes of gynaecological cancers are not known, it is important
to identify women who may be at a higher risk of developing these cancers and then
implement strategies that may assist in prevention and early intervention. The
Gynecologic Cancer Foundation in the United States stated:
Diet, exercise and lifestyle choices play a significant role in
the prevention of cancer. Additionally, knowing your family history can
increase your chance of early diagnosis and can help you take action toward
prevention. Screening and self-examination conducted regularly can result in
the detection of certain types of gynaecologic cancers in their earlier stages,
when treatment is more likely to be successful and a complete cure is a
possibility.[4]
The symptoms of gynaecological cancers
1.18
Most gynaecological cancers do not show early signs or symptoms. Symptoms
often appear late in the condition and have been described as vague and ill-defined.[5]
Many of the identified symptoms of gynaecological cancers are common and can be
similar to those occurring in women during their monthly menstrual cycle and may
also suggest the presence of other medical conditions.
1.19
Commonly identified symptoms for gynaecological cancers are:
- abdominal bloating and/or feeling full;
- appetite loss;
- excessive tiredness and fatigue;
- unexplained weight gain;
- heartburn;
- increased swelling of the lower abdomen without weight gain
elsewhere;
- increased swelling of the lower abdomen which does not improve
with diet or exercise;
-
a lump or mass in the abdomen, especially the lower abdomen;
- lower abdominal or pelvic pain that does not settle quickly and
simply;
- feelings of pressure on the bowel or bladder and a feeling that
the bowel or bladder cannot be completely emptied (constipation/urinary
frequency);
- abnormal bleeding from the vagina, especially bleeding after the
menopause;
- bleeding after intercourse;
- pain during intercourse;
- unusual vaginal discharge;
-
leg pain or swelling; and/or
- low back pain.[6]
1.20
The need for education to inform women, the broader community and the
medical community of the symptoms of gynaecological cancers is discussed in Chapters 5
and 6.
Statistics on gynaecological cancers in Australia
1.21
The Australian Institute of Health and Welfare's (AIHW) most recently
published report Health System expenditures on cancers and other neoplasms
in Australia (May 2005) records data for the year 2000-2001.[7]
The fact that the most recent figures are five years old at publication creates
difficulties when using these statistics as the basis for public policy
decisions.
1.22
Evidence presented during the inquiry identified a number of difficulties
relating to adequate data collection, including inconsistent cancer registry
data and the ad hoc collection of gynaecological cancer data. Particular inadequacies
were identified for Indigenous women and women from culturally and linguistically
diverse populations. Data collection is discussed in Chapter 4.
Incidence of gynaecological cancers
1.23
In Australia in 2001, 3,886 women developed gynaecological cancers
making this as a group of cancers the third most common for women, behind
breast (11,791), colorectal cancer (5,883) and ahead of melanoma (3,861) and
lung (2,891).[8]
1.24
The AIHW commented that for the period 1991 to 2001, there was:
- an 8 per cent increase overall in new cases of gynaecological
cancers;
- a 31 per cent increase of the number of new cases of cancer of
the uterus;
- a 23 per cent increase of the number of new cases of ovarian
cancer and other cancers of the female genital organs;
- a 18 per cent increase of the number of new cases of cancer of
the vulva, vagina and placenta; and
- a 33 per cent decrease of the number of new cases of cervical
cancer.[9]
Table 1: Number New Cases of
each Gynaecological Cancer, 1998 - 2001
|
|
1998
|
1999
|
2000
|
2001
|
|
Vulval
|
211
|
200
|
203
|
252
|
|
Vaginal
|
56
|
73
|
71
|
62
|
|
Cervical
|
855
|
794
|
754
|
735
|
|
Uterine
|
1397
|
1434
|
1580
|
1537
|
|
Ovarian
|
1232
|
1218
|
1263
|
1248
|
|
Other
Gynaecological
|
50
|
67
|
58
|
52
|
Source:
Submission 24, p.5 (ASGO).
Projections for new cases of
gynaecological cancers
1.25
With an increase in the age of the population, the overall number of new
cases of gynaecological cancers is projected to increase by almost 15 per cent
from 3,886 in 2001 to 4,487 in 2011.[10]
1.26
The AIHW project that the incidence of gynaecological cancer as a group
will slowly decline over time as a result of the decrease in the incidence of
cancer of the cervix. The improvement in the cervical cancer incidence rate has
been attributed in part to the National Cervical Screening Program and the
early detection of cervical cancer.
1.27
In fact, cancer of the cervix is the only gynaecological cancer for
which the expected number of new cases is projected to decrease even with the
expected ageing of the population. The number of new cases reported in 2001 was
735, which is projected to decrease by 37 per cent to 461 by 2011.[11]
1.28
The AIHW has projected the incidence of new cases of gynaecological
cancers in 2006 and 2001 and these figures are detailed in Table 2.
Table 2: AIHW projection of
incidences of gynaecological cancers
|
|
2006
|
2011
|
|
Gynaecological cancer
|
Number
|
|
Cervical cancer
|
582
|
461
|
|
Cancer of uterus
|
1738
|
1967
|
|
Ovarian cancer and other unspecified cancers of the female genital
organs
|
1465
|
1645
|
|
Cancer of vulva, vagina
and placenta
|
367
|
414
|
|
Total
cancers of female genital organs
|
4152
|
4487
|
|
|
Per cent
|
|
Cervical cancer
|
14.0
|
10.3
|
|
Cancer of uterus
|
41.9
|
43.8
|
|
Ovarian cancer and other unspecified cancers of the female genital
organs
|
35.3
|
36.7
|
|
Cancer of vulva, vagina
and placenta
|
8.8
|
9.2
|
|
Total
cancers of female genital organs
|
100.0
|
100.0
|
Source:
Submission 3, p.1 (AIHW).
Deaths from gynaecological cancers
1.29
When considering mortality from gynaecological cancers, the AIHW stated:
The risk of developing a malignant gynaecological cancer is 1 in
34 by 75 years of age and increases to 1 in 23 by 85 years of age.
The risk of dying from a malignant gynaecological cancer is 1 in 103 at 75 years
of age and rises to 1 in 55 by 85 years of age.[12]
1.30
The Sydney Gynaecological Oncology Group commented on the high mortality
rate for gynaecological cancers compared with breast cancer.
The number of women dying from gynaecological cancers is
disproportionately high compared to breast cancer which only had a comparative
22% mortality rate in 2001. Much of this effect is from ovarian cancer with a
66% death rate in the same period.[13]
Table 3: Deaths from
gynaecological cancers
|
|
1991
|
2001
|
2004
|
|
Gynaecological cancer
|
Number
|
|
Cervical cancer
|
336
|
262
|
212
|
|
Cancer of uterus
|
257
|
293
|
327
|
|
Ovarian cancer and other unspecified cancers of the female genital
organs
|
728
|
846
|
851
|
|
Cancer of vulva, vagina
and placenta
|
72
|
117
|
89
|
|
Total
cancers of female genital organs
|
1393
|
1518
|
1530
|
|
|
Per cent
|
|
Cervical cancer
|
24.1
|
17.3
|
14.3
|
|
Cancer of uterus
|
18.4
|
19.3
|
22.1
|
|
Ovarian cancer and other unspecified cancers of the female genital
organs
|
52.3
|
55.7
|
57.5
|
|
Cancer of vulva, vagina
and placenta
|
5.2
|
7.7
|
6.0
|
|
Total
cancers of female genital organs
|
100.0
|
100.0
|
100.0
|
Source:
Submission 3, p.2 (AIHW).
Survival rates for women with
gynaecological cancers
1.31
The AIHW provided the life expectancy for women (relative survival) five
years after diagnosis for the following gynaecological cancers:
- endometrial – 81.4 per cent;
- cervical cancer – 74.6 per cent; and
- ovarian cancer – 42 per cent.[14]
1.32
The Garvan Institute of Medical Research provided a comparative relative
survival rate for breast cancer of 84 per cent and commented that
ovarian cancer was less than half this figure.[15]
Conclusion
1.33
Some gynaecological cancers remain a mystery with an absence of
knowledge and definitive understanding of the causes, signs and symptoms. The
incidence of these types of cancer (with the exception of cervical cancer) is
projected to increase in years to come. Although the Committee heard that Australia
is performing well when compared internationally, the fact remains that in 2004,
1,530 Australian women died as a result of gynaecological cancers and this
figure will most likely increase if further advancements in screening,
treatment and wider health support programs are not found.
Navigation: Previous Page | Contents | Next Page