Stillbirth reporting and data collection
4.1
There is no systematic approach to reviewing and reporting stillbirths
across Australia. This lack of standardisation and coordination has significant
implications for research and education aimed at preventing future stillbirths.
4.2
The collection and analysis of data to determine trends in the rate,
risk factors and underlying causes of stillbirth over time is important for
understanding how stillbirth rates may be reduced, and provides direction for
future research, education and preventive efforts. Data collection
needs to encompass a wide range of factors in order to inform stillbirth
prevention strategies.
4.3
The World Health Organisation (WHO) estimates that around 60 per cent of
countries do not have adequate systems for counting births and deaths, and has
produced Making Every Baby Count, a guide for the audit and review of
stillbirths and neonatal deaths.
By counting the number of stillbirths and neonatal deaths,
gathering information on where and why these deaths occurred and also by trying
to understand the underlying contributing causes and avoidable factors,
health-care providers, programme managers, administrators and policy-makers can
help to prevent future deaths and grief for parents, and improve the quality of
care provided throughout the health system.[1]
4.4
The current process to develop a National Strategic Approach to
Maternity Services, initiated by the Australian Health Ministers' Advisory
Council (AHMAC), acknowledges that a national perinatal audit program is yet to
be implemented.[2]
4.5
This chapter discusses the quality and scope of stillbirth reporting and
data collection, and considers inconsistencies, gaps, costs, access and
timeliness in Australia's stillbirth reporting and data collection system, as
well as issues relating specifically to autopsies and other post-mortem
investigations.
Quality and scope of data
4.6 The Department of Health funds the Australian Institute of Health and
Welfare (AIHW) to collect data from each jurisdiction as part of the National
Perinatal Data Collection (NPDC), undertake data analysis and prepare reports
on perinatal deaths, including stillbirths. The AIHW has produced Stillbirths
in Australia, 1991−2009,
and publishes biennial reports on perinatal mortality. The most recent detailed
data available is for 2013−14.[3]
4.7
The most recent consolidated report, Perinatal Deaths in Australia
1993−2012,
provides an overview of the characteristics and causes of stillbirth and
neonatal deaths in Australia at a population level, and identifies trends and
changes in perinatal mortality over time.[4]
4.8
In its 2009 review of the Maternity Services Plan, the Department of
Health identified that data gaps were a significant issue, and established the
National Maternity Data Development Project (NMDDP) to develop a nationally
consistent maternal and perinatal data collection.
Stage 1 (2011−13)
prioritised data gaps and inconsistencies in the existing NPDC, and included a
National Perinatal Mortality Data Reporting Project to identify options for
collecting and reporting national perinatal mortality data. Stages 3 and 4 of
the NMDDP (2015−17)
included the development of nationally consistent maternal and perinatal
mortality data collection in Australia with standardised data specifications,
annual reporting and data base development.[5]
4.9
However, a number of witnesses and submitters identified continuing
problems affecting the quality, scope, timeliness and accessibility of
stillbirth data.
Inconsistencies in perinatal data
collection and reporting
4.10
The Centre of Research Excellence for Stillbirth (Stillbirth CRE) stated
that the current national practice for stillbirth reporting data collection is
'suboptimal', with significant implications for the quality of research
outcomes and policy decisions.
Major impediments to timely, quality data to inform effective
prevention strategies for stillbirth include significant duplication of effort
and disparate approaches across and within states and territories.[6]
4.11
The National Perinatal Epidemiology and Statistics Unit (NPESU) at the
University of New South Wales (UNSW) reported on the difficulty of identifying
research priorities when access to national data is 'highly constrained' and
national reporting lacks detailed results.[7]
The lack of consistent ongoing funding for epidemiological
research and reporting of stillbirth in Australia is hampering the ability to
undertake this important research in Australia. The current restrictive
processes for standardised national collection of data about pregnancy and
birth have resulted in a national reporting system that is unresponsive to
change, is delayed and lacks clinically meaningful and relevant information to
assist clinicians in making changes to reduce the rate of preventable
stillbirth. Improvements in the timeliness of and access to national data on
pregnancy and birth are vital if we are to improve outcomes for mothers and
babies and reduce the rate of preventable stillbirth in Australia.[8]
4.12
The NPESU also noted that it had prepared a report for AIHW in 2016,
although this report has not been published. The report examined options for
improving perinatal mortality data collection and reporting in Australia,
including consultation with perinatal data custodians.[9]
Stillbirth datasets
4.13
Australia has two national datasets that record stillbirth in different
ways and produce different results, as follows:
- The AIHW is responsible for collating 'health' data on stillbirths in
Australia. The AIHW collates data in the NPDC and the National Perinatal
Mortality Data Collection (NPMDC), drawn from state and territory health authorities
under individual data agreements between the AIHW and each state and territory.[10]
-
The Australian Bureau of Statistics (ABS) sources data from state and
territory registries of Births, Deaths and Marriages and tabulates information
on perinatal deaths, including stillbirths, as part of the Causes of Death,
Australia (ABS Cat No. 3303.0) report, which is released annually.[11]
4.14
In addition, the National Hospital Morbidity Database is a collection of
electronic confidential summary records in public and private hospitals in
Australia, compiled from data supplied by state and territory health
authorities.[12]
4.15
These large population datasets are important for stillbirth research,
particularly for undertaking large-scale epidemiological research using modern
big-data analytics to determine why stillbirths occur and how to prevent them.
However, data collected by the ABS generally shows lower rates of stillbirths
than that collected by the AIHW, owing to the way that stillbirth is, or is
not, accounted for in births and deaths in individual states and territories.
For example, the ABS reported 23.8 per cent fewer stillbirths for 2013−14 than reported by
AIHW.[13]
As NPESU noted:
Rates of stillbirth vary depending on which national source
is used, with the ABS data known to significantly under-report the rate of
stillbirth in Australia[14]
4.16
The under-reporting of stillbirths by the ABS is largely attributable to
the two-step verification process required to fully register a stillbirth: the
Medical Certificate of Cause of Perinatal Death issued by the attending
clinician, and a statement from the parents. If only one notification is
received, a partial registration is recorded.[15]
Mr James Eynstone-Hinkins, Director, Health and Vital Statistics, ABS, outlined
the process as follows:
We collect information on all stillbirths registered through
the registries of births, deaths and marriages in line with the same method
used internationally for collecting information on perinatal deaths. The
registration criteria in Australia for stillbirths are 20 weeks gestational age
or 400 grams birth weight. That aligns with the Australian criteria and the ABS
inclusion criteria. The causes of stillbirths and neonatal deaths are recorded
on the medical certificate of cause of perinatal death. This captures the main
condition in the infant and the main condition in the mother as well as any
other relevant conditions. Causes are coded in accordance with the
international classification of diseases, according to coding rules governed by
the World Health Organization and used by WHO member states. The data that we
capture is released approximately nine months after the end of a reference
period, which roughly equates to a calendar year. That is released as aggregate
data as part of the national causes of death data set.[16]
4.17
The statutory instruments and registration practices related to
registration of births and perinatal deaths vary between jurisdictions. There
are also variations in the reported causes of stillbirth. ABS data shows the
number of unexplained stillbirths as three times that reported by AIHW (ABS, 64
per cent compared to AIHW, 20 per cent) as a result of ABS using information on
the death certificate at the time of stillbirth and prior to the result of any
investigation into the causes. AIHW data, on the other hand, is based on
classification of causes following review of all available post-mortem
investigations.[17]
Mandatory and voluntary items
4.18
Some data in the NPDC is mandated by the National Health Information
Standards and Statistics Committee for collection under agreements between the
Commonwealth and each state/territory as part of the National Minimum Data Set
(NMDS).[18]
4.19
A national committee, the National Perinatal Data Development Committee,
comprising the PDC custodians from each state and territory and the AIHW,
manage what is included in the NPDC and which data items are mandated for
collection in all jurisdictions. Each jurisdiction must agree to add a new item
and commence collection and reporting otherwise data are collected on a
voluntary basis and may differ between jurisdictions.
4.20
The AIHW noted that the Perinatal Mortality Committee uses data from
jurisdictional perinatal mortality committees about the circumstances of a
baby's death, the social history of the family and the professional care of the
mother, and advised that it is working towards including this data in national
reports 'as the quality of the data collected improves'. However, it also noted
a high proportion of responses for certain items are 'not stated' because they
are of a voluntary nature.[19]
4.21
Dr Fadwa Al-Yaman, Group Head, Indigenous and Maternal Health Group,
AIHW, explained why there are delays in adding a new item to the national
collection. The AIHW is required to determine what data are clinically relevant
and appropriate by consulting with clinical experts, and defining the
additional items based on national and international standards and guidelines. The
AIHW then seeks agreement with the jurisdictions and clinical experts through a
national committee. Once agreed, the new specifications are sent to the states
and territories. In some jurisdictions, the new items are already collected. In
other cases, the data may need to be collected 'from scratch', requiring
changes to that jurisdiction's system of data collection. The AIHW allows six
months for this new information to be collected, but delays in receiving the
new data from the states and territories may lead to delayed publication of the
national dataset.[20]
4.22
The NPESU argued that the information used for national stillbirth and
neonatal death reporting 'is missing vital information to allow for
comprehensive analysis, due to a lack of mandated standardised data items'.[21]
Inconsistent definitions
4.23
Within Australia, registration of stillbirths occurs at a state and
territory level, and each jurisdiction has its own register of births and
deaths and legislation defining what is registered as a birth or death in ABS
data. There is, for example, no standardised definition of what constitutes a 'live
birth' across the jurisdictions, making it difficult to distinguish between a
termination of pregnancy, a stillbirth and a live birth.[22]
4.24
All states and territories, except for Western Australia (WA), register
stillbirths only as births. WA registers a stillbirth as both a birth and a
death. South Australia (SA) does not include termination of pregnancy after 20
weeks in its legislative definition of 'birth'.[23]
4.25
Victoria is the only state that offers access to late term termination
between 20−24
weeks on request (without a referral or doctor’s approval).[24]
This means the rate of stillbirth for Victoria appears high in comparison to
other jurisdictions (9.1 per 1000 births in 2013−14,
compared to 7.1 per 1000 for the whole of Australia).[25]
4.26
In addition, lower populations and smaller numbers of births and
stillbirths can lead to significant variations in stillbirth rates over time,
which may be misleading. This is particularly relevant in considering the
higher rates of stillbirth in Aboriginal and Torres Strait Islander and
culturally and linguistically diverse (CALD) populations in Australia.[26]
4.27
There is also a lack of consistency in how risk factors are classified
across different jurisdictions, suggesting that this may be the result of
different data and evaluation processes being used.[27]
4.28
As a result, stillbirth data are recorded differently making it
difficult to determine the rate of stillbirths across Australia. This is
especially problematic where a woman moves from her place of residence in one
jurisdiction in order to give birth in another jurisdiction.[28]
4.29
This issue is noted in the Australian government's latest report on
Sustainable Development Goals Indicators.
Various definitions are used for reporting and registering
perinatal deaths in Australia. The National Perinatal Data Collection defines
perinatal deaths as all fetal deaths (stillbirths) and neonatal deaths (deaths
of liveborn babies aged less than 28 days) of at least 400 grams birthweight or
at least 20 weeks’ gestation. Fetal and neonatal deaths may include late
termination of pregnancy (20 weeks or more gestation). Perinatal and fetal
death rates are calculated using all live births and stillbirths in the
denominator. Neonatal death rates are calculated using live births only.
Neonatal deaths may not be included for babies transferred to another hospital,
re-admitted to hospital after discharge or who died at home after discharge.
The Australian Institute of Health and Welfare (AIHW) has established a
separate National Perinatal Mortality Data Collection to capture complete
information on these deaths.[29]
4.30
The AIHW divides perinatal outcomes into three categories: stillbirths,
live born neonatal survivors, and neonatal deaths, as follows:
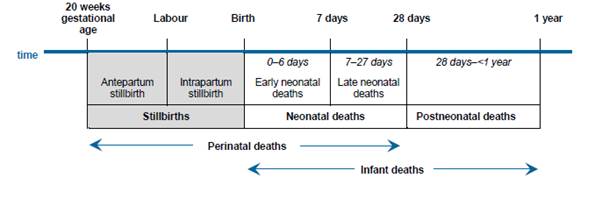
Figure 4.1: Perinatal death periods
for reporting in Australia[30]
4.31
Stillbirth CRE argued that the lack of consistent definitions for many
data items impacts on the accuracy of comparisons across jurisdictions and the
capacity to identify key outcomes. It also leads to a time lag of two to three
years between data collection and publishing in state/territory and national perinatal
mortality reports.[31]
Inadequate reporting standards
4.32
International studies have shown that inadequate information relating to
the timing of the stillbirth and other details in relation to pregnancy and
birth, maternal risk factors, obstetric and other conditions limits the value
of data for evaluating and implementing preventive strategies.[32]
4.33
According to Australian researchers, the data collected by the AIHW are
not comprehensive, consistent nor detailed enough to enable the information to
be used in meaningful ways to improve clinical care. This is due to a number of
factors, including that a number of items in the data collections are voluntary
(as noted above), which correlates with a higher rate of 'unknown' or
'unspecified' for those items.[33]
4.34
Stillbirth Foundation Australia highlighted the need to break Australian
stillbirth data down to a more granular level of analysis in order to
understand trends, and to make this data available to the private sector,
researchers and relevant organisations to encourage a more collaborative
environment.[34]
4.35
Having access to granular data is particularly important in giving a
greater understanding of where research needs to be concentrated, particularly
amongst rural and remote, Aboriginal and Torres Strait Islander and women from
CALD backgrounds for whom there is an elevated risk of stillbirth and other
adverse pregnancy outcomes.[35]
4.36
Gestational age at birth, for example, is only reported nationally in
completed weeks of gestation, which is an impediment to researching the impact
of gestational age. '[M]ortality differences between 41.0 weeks' and 41.6
weeks' are of clinical significance but treated the same in a data collection
that records only "completed weeks"', that is, both are recorded in
data collections as 41 weeks' gestation.[36]
4.37
The NPESU noted that the lack of granular data has disguised the fact
that there have been some improvements in stillbirth trends amongst particular
age groups.
...national reporting indicates that there has been relatively
little change in the overall stillbirth rate in Australia over the past 20
years...However, more in depth statistical analysis undertaken by the NPESU...has
shown that improvements have been made in the risk of stillbirth at later
gestational age groups, and the inclusion of terminations of pregnancy and
reporting overall rates of stillbirth (rather than at different stages of
pregnancy) in national statistics has masked some of the inroads gained.[37]
4.38
The Royal Australian and New Zealand College of Obstetricians and
Gynaecologists (RANZCOG) considered that '[i]t is a serious deficiency of the
national perinatal data set (and some state perinatal data sets), that maternal
height and weight is not recorded'.[38]
RANZCOG submitted that such customisation of data could be used to better
predict the risk of fetal growth restriction, for example, and that 'not
collecting critical data impairs important research'.[39]
4.39
RANZCOG also noted, in relation to antenatal testing of fetal genetic,
chromosomal and structural conditions, that there is an 'absence of national
data collection in this critically important area of maternity care...[which] can
assist in the prevention of mortality and long-term morbidity through measures
being put in place around birth or early in the neonatal period'. Given that fetal growth restriction is the single largest cause of
unexplained stillbirth, RANZCOG argued there was an urgent need to adopt
'severe intra-uterine growth restriction in a singleton pregnancy undelivered
by 40 weeks' as a core maternity indicator in the National Core Maternity
Indicators.[40]
4.40
Professor Euan Wallace, Carl Wood Professor and Head of Department of
Obstetrics and Gynaecology, Monash University, stated that women from migrant
backgrounds are significantly under-represented in stillbirth data, including
second generation South-East Asian women who migrated to Australia following
warfare in their countries and who are recorded as Australian.
Those women are disproportionately represented in our
stillbirth data, yet our data collection systems are blind to maternal and
paternal ethnicity. We collect country-of-birth information of mothers but we
don't collect ethnicity.[41]
4.41
Dr Jane Warland also noted that data collected on stillbirth generally omitted
information about the father, even though he contributed half of the baby's DNA
and his ethnicity and age are likely to be important.[42]
Lack of data for rural, regional
and remote Australia
4.42
There are almost seven million people living in rural, regional and
remote Australia yet, as the AIHW review found, babies born to mothers living
in these areas are 65 per cent more likely to die during the perinatal period
than babies born to mothers living in major cities or inner regional areas.
Indeed, the further away women are from a major city, the higher the rate of
stillbirth.[43]
4.43
The National Rural Health Alliance called for improved data collection
quality, consistency and dissemination so that it can be used to improve rural
and remote maternal health outcomes and reduce perinatal deaths as well as
improving quality and safety of care, identifying lessons learned and
translating research into clinical practice and shared knowledge.[44]
4.44
Ms Victoria Bowring, Chief Executive Officer, Stillbirth Foundation
Australia, pointed to the need for more granular data in order to be able to
concentrate research in areas where there is inadequate data. Rural and remote
communities do not have access to the same level of health care as others, yet
there is no data to establish the extent to which such communities are at
higher risk of stillbirth.
It's one thing to submit a figure that is the sum total for a
nation at the end of a five-year period, but, if we had access to where these
are occurring—family history, background, location and all of those finer
details—it gives a greater understanding of where the research needs to be
concentrated.[45]
Difficulty and cost of accessing
data
4.45
The AIHW does not own the data contained in the NPDC, which is a collation
of all the state and territory Perinatal Data Collections (PDC, also known as
Midwives Data Collections). The data are therefore owned by the jurisdictions.[46]
4.46
The NHMRC has an Open Access Policy which aims to 'mandate the open
access sharing of publications and encourage innovative open access to research
data'.[47]
Recipients of NHMRC grants must comply with this policy.
4.47
However, given the relatively low numbers of stillbirth, researchers
wishing to access stillbirth data on a national scale need to seek agreement
from each jurisdiction each time they require it. This can be a lengthy and
costly process that extends beyond the time available to researchers dependent
upon three-year research funding cycles.[48]
4.48
According to the NPESU, the cost of accessing data ranges from $12 000
to $25 000, depending on the nature of the data requested. In
addition, it can take three to five years just to obtain the necessary
jurisdictional, national and ethical approvals required by AIHW to access
national perinatal data.[49]
4.49
Similarly, the Western Australian Perinatal Epidemiology Group noted
that the 'costs of obtaining de-identified linked data from government are
increasing and are approximately 10 per cent of a requested research
budget...Preferably, provision of [this] data for research should be considered a
core government service and therefore not cost recovered', as is the case in
the United States of America (USA).[50]
4.50
Mrs Ellana Iverach noted that the information derived from medical
reviews and investigations of a stillbirth was difficult to locate, and that it
should be more easily accessed so that it can be made available to researchers
and other interested parties.[51]
4.51
The NPESU pointed to the Vital Statistics Online Data Portal used in the
USA which offers a best-practice perinatal data collection model that is a far
simpler and cheaper for researchers to access.
The tortuous process for accessing national perinatal data in
this country stands in stark contrast to access to perinatal data in the USA
where birth, cohort and period linked birth and infant death, cause of death
and fetal death data are made available for independent research and analyses
and can be downloaded free of charge. The level of detail exceeds that
available in Australia.[52]
Timeliness of data
4.52
Access to timely, high-quality data on causes and contributing factors
to stillbirth are crucially important, not only for helping bereaved parents to
understand what happened and to plan for future pregnancies, but also to inform
the development of targeted prevention strategies.[53]
4.53
However, several submitters raised the negative impact of delayed access
to data on the ability of researchers to identify and address emerging issues
relating to stillbirth.[54]
The NPESU noted the long delays involved in adding new data items to the NPDC.
While having a NMDS is vital to ensuring consistency of
reporting across the country, the process of adding new data items to the
collection, gaining agreement from all jurisdictions and proceeding through the
data development processes means it can take up to 5 years or longer before an
item is mandated for collection and then a further 2 years before it might
appear in a national report. This is very relevant to the issue of reporting of
stillbirth data in Australia.[55]
4.54
Based on information reported to the AIHW by states and territories,
most stillbirths in Australian hospitals are reviewed by a hospital-level
committee and then a jurisdiction-level perinatal mortality review committee.[56]
4.55
However, the AIHW cited delays in provision of data by states and
territories as the reason for the delay in reporting, and indicated that it
would publish detailed data from 2015 by the end of the 2018 calendar year with
the intention to update perinatal deaths data online annually from 2019.[57]
4.56
In 2016, the NHMRC published Principles for Accessing and Using Publicly
Funded Data for Health Research. The principles were developed to 'improve the
consistency and timeliness of data available to researchers'.[58]
4.57
Professor Wallace noted that, whilst Australia has a secure system in
place for sharing sensitive data known as Secure Unified Research Environment
(SURE), the timeliness of data is inhibited by a lack of resources available for collating and linking perinatal data.[59]
4.58
Timely data are also considered crucial for identifying areas of substandard
care that may contribute to stillbirth.
4.59
Stillbirth CRE reported that it had developed, in partnership with the
Victorian Department of Health, an online system for national perinatal
mortality audits designed to enhance investigation and reporting of stillbirths
by providing timely data that will enable substandard care to be identified and
addressed. 'In both New Zealand and the United Kingdom (UK) national audit data
and timely feedback has led to reduced perinatal deaths through quality
improvement.'[60]
Linked datasets
4.60
Associate Professor Georgina Chambers, Director, NPESU, Centre for Big
Data Research in Health and School of Women's and Children's Health, Faculty of
Medicine, UNSW, noted that the NPESU has analysed stillbirth and neonatal data
across jurisdictions and identified the discrepancies between the different
datasets. She recommended that Council of Australian Governments should
prioritise the harmonisation, sharing and centralisation of health data to
establish comprehensive, standardised NPMDC.
Because Australia is a federation of states and territories,
we understand it is challenging to bring together a standardised set of data
items related to perinatal deaths that can be used not only by health systems
but also by researchers. It takes five years for a new mandatory item to be
added to the state perinatal data collections and at least another two for that
item to be reported on. A comprehensive perinatal mortality data collection
should routinely link to other datasets—such as the various registries of
births, deaths and marriages—to improve surveillance and should be integrated
with the national maternity mortality audit tool that was developed by the
Mater Research Institute and PSANZ. The NPESU laid the basis for comprehensive
data collection when we prepared the first perinatal mortality report in 2016.
Creating such an important dataset would not be difficult; it just takes
commitment and leadership from all involved.[61]
4.61
The AIHW noted that data gaps in the perinatal mortality collection
could be addressed by linking data to established collections, such as linking Medicare
Benefits Schedule (MBS), Pharmaceutical Benefits Scheme (PBS) and NPDC data.[62]
4.62
The Population Health Research Network (PHRN), funded under the National
Collaborative Research Infrastructure Strategy to build linkages between
datasets in privacy-preserving ways, advised that seven of the eight states and
territories routinely link perinatal and death data to other administrative
data collections. These linked collections include MBS and PBS data, as well as
clinical trial and other researcher datasets, and recommended that researchers
should be made more aware of these linked, multi-jurisdictional resources.[63]
4.63
The PHRN noted that a more detailed understanding of stillbirth could
also be gained by linking death and perinatal data with data from other sources,
such as hospital admissions and emergency department admission. However,
several challenges remain in achieving coordinated datasets across
jurisdictions as a result of different legislation and policies and reluctance
by some jurisdictions to share identifiers across borders. The PHRN noted that
a project is underway that may address these issues and seeks to improve
linkages between state/territory data collections and the Commonwealth data
collections through the AIHW.[64]
To get the full picture on health in Australia we need to be
able to bring those together. Australia can already bring that data together,
but it generally does it in a way that we would describe as create and destroy.
Those linkages are not maintained. The good news is that we are making good
progress with systematically linking that data, and I think it won't be too
long before we have that data available to researchers.[65]
4.64
Ms Belinda Jennings, Senior Midwifery Advisor, Policy and Practice,
Katherine Hospital noted that, whilst midwives across Australia contribute to a
minimum perinatal dataset, they also collect data on hundreds of other items
during the course of a pregnancy. That dataset, however, is not linked to the NPDC.
The feedback from some midwives is that they don't want to be
collecting data twice, but the benefit of the perinatal death data collection
tool is that it is an all-encompassing one-stop shop which incorporates
contributing factors, classifications and categorisations. So they sit parallel
to one another, with equal importance in the arena of stillbirth,...It's a
shame they're not going to talk to one another, because otherwise you could
dump them there to export a lot of the information from midwives.[66]
4.65
The Australian Longitudinal Study on Women's Health (ALSWH), a
longitudinal population-based survey examining the health of over 58 000
Australian women, is funded by the Commonwealth Department of Health and
managed by the universities of Newcastle and Queensland. The study includes a
survey of women's experience of stillbirth throughout their reproductive years.
4.66
ALSWH links women's survey data to administrative datasets providing
perinatal data (with provision for participants to opt out), and makes the data
freely available to researchers. It also sources hospital admission and cancer
registry data at the state/territory level and MBS and PBS data at the national
level.[67]
4.67
If made mandatory, linking the different datasets across states and
territories, and integrating them with the perinatal data, PBS data, MBS data,
and Perinatal Data Collections would yield important information including the
financial impact of stillbirth on the public health system.[68]
Improving perinatal reporting and
data collection
4.68
In order to address inconsistencies and delays in perinatal data
reporting, and ensure that timely and consistent data are available to
researchers and policymakers, Stillbirth CRE recommended the following
strategies:
- introduction of a standardised national electronic reporting
system to collect 'real-time' data of all births across Australia, including
agreement on a single definition of stillbirth and the reporting systems to be
used;
-
annual reporting on perinatal deaths nationally, with a focus on
stillbirths and including Indigenous and other high risk groups, to enable the
impact of programs and policies to be monitored for effectiveness;
-
inclusion of stillbirth rates as a key performance indicator in
all state and territory annual perinatal outcomes reports; and
-
hospital level audits of stillbirths and neonatal deaths to
identify factors relating to care, to be included in national, state and
territory reporting that informs improvements in clinical practice.[69]
Perinatal mortality audits
4.69
In its report on perinatal deaths in 2013−14
the AIHW noted that, of the 6037 perinatal deaths that occurred, only 235 cases
were reviewed by a jurisdictional perinatal review committee to consider
possible contributing factors that would assist in identifying systemic issues
affecting the perinatal mortality rate. Of the 235 cases reviewed, 99 were
found to have contributing factors including professional care (58 per
cent) or to the situation of the mother, her family or social situation
(39 per cent), with 38 cases having factors likely to have significantly
contributed to the adverse outcome.[70]
4.70
Several submitters and witnesses called for a national policy on the
conduct of stillbirth autopsies and perinatal mortality reviews as well as the
collection and sharing of data.[71]
4.71
The Clinical Practice Guideline for Care Around Stillbirth and
Neonatal Death, developed by the Perinatal Society of Australia and New
Zealand (PSANZ) and Stillbirth CRE, encourages clinicians in maternity services
to standardise investigation, classification and reporting of stillbirths in
order to improve the quality of data in Australia. However, Stillbirth CRE
noted that application of this Guideline has been variable across Australia.[72]
4.72
Ms Natasha Donnolley, who co-authored the first report on perinatal
deaths in Australia, was critical of the lack of a national approach to
perinatal mortality audits. She noted that, whilst there is now an electronic
data collection tool available to jurisdictions, only Victoria has been active
in this area.[73]
4.73
Victoria has a long tradition of individual case review through the
Consultative Council of Obstetric and Paediatric Mortality and Morbidity, an
independent legislative body charged with reviewing all perinatal, child and
adolescent deaths. Recommendations arising from these reviews are used to
direct improvements in healthcare provision.
4.74
Victoria also undertakes annual reporting of Victorian Perinatal
Services Performance Indicators which compares identifiable hospital data
on outcomes for mothers and newborns against 10 safety and quality indicators. Making
this information publicly available to clinicians and families has resulted in
a 35 per cent improvement in the detection of fetal growth restriction.[74]
4.75
Ms Donnolley noted that there has not been a state-wide audit of
perinatal mortality in NSW, and it is therefore not possible to learn lessons
about causes and prevention of stillbirth.
Other states have recently commenced piloting an electronic
perinatal mortality audit tool but a national approach is urgently needed for
consistency and for maximum benefit. Parents deserve to know that when they
consent to post mortem examinations, that the information is contributing to a
full investigation of their baby’s death and that it will be used to the
benefit of others as well as to find their own answers.[75]
4.76
Several witnesses noted that New South Wales (NSW) public hospitals are
required to prepare a 'root cause analysis' undertaken by a group of
independent expert clinicians external to the hospital where a stillbirth has
occurred. However, this is only undertaken by private hospitals on a voluntary
basis. In addition in NSW, which has almost one-quarter of all
stillbirths in Australia, the perinatal mortality review committee has not
undertaken a perinatal mortality review for more than four years, and its
policy is more than seven years out of date.[76]
4.77
The committee also heard evidence from bereaved parents that there was
no standard information collected from them in relation to their experience of
the pregnancy in the period immediately preceding the stillbirth, and no
clarity as to how information obtained through a review of the stillbirth was
compiled or subsequently used by researchers or clinicians.[77]
4.78
One submitter proposed giving a survey to all parents after their child
is stillborn which, when combined with data from the hospital, could be made
widely available to researchers, medical professionals and families to help
them better understand risks and methods of prevention.
It is not enough for research to be published in obstetric
and midwifery journals. Women may see a whole range of medical professionals
during their pregnancy, and each have a role to play in ensuring the safety of the
woman and her baby.[78]
Successful international models
4.79
Several witnesses commented on the success of overseas models of
stillbirth data reporting and collection, with evidence indicating that they
had contributed to a significant reduction in the rate of stillbirth in those
countries.
4.80
Professor Jason Gardosi, Director of the Perinatal Institute in the UK,
reported on the success of a stillbirth prevention program developed by the
Perinatal Institute using detailed case reviews and analysis of regional
maternity data.
4.81
The GAP program, which has now been implemented in over 80 per cent of
UK hospitals in the National Health Service, is a comprehensive training and
audit program drawing on data collected in relation to the mother's height,
weight, previous pregnancies and ethnicity to produce a core dataset of
maternal characteristics. It also enables the generation of customised
antenatal growth charts (GROW) to assist obstetricians, midwives and
ultrasonographers in undertaking antenatal assessments, and is credited with
reducing stillbirth rates by 23 per cent over the last six years.[79]
4.82
The Perinatal Institute has also been commissioned to roll out the GAP
program in New Zealand, and it has produced an Australian version. The
customised GROW chart and calculators are already being used by clinicians in
some Australian states and territories, with evidence suggesting that they are
helping to improve antenatal identification of babies at risk due to fetal
growth restriction. The Perinatal Institute (UK) concluded that:
...a significant and sustained impact on stillbirth prevention
will require a co-ordinated, intensive yet affordable programme, modelled on
experience elsewhere and adapted to Australian circumstances.[80]
4.83
The MBRRACE-UK program is an initiative established in 2012 and administered
by the Healthcare Quality Improvement Partnership to conduct surveillance and
investigate causes of maternal deaths, stillbirths and infant deaths. The
program involves confidential enquiries into aspects of perinatal death
including stillbirths, and has a collaborative and multi-jurisdictional
approach. In 2016 the rate of perinatal mortality had decreased overall, and
the stillbirth rate for twins had nearly halved since 2014.[81]
4.84
The Netherlands has implemented a system of timely and consistent data
collection and review, resulting in the rate of stillbirth being reduced by
nearly 60 per cent.
The Netherlands system incorporates about seven different
elements but it incorporates staff education, it incorporates patient
education, it incorporates central recording systems with central reporting and
it requires that to be monitored and for people to be accountable for it. So
the hospitals are accountable for their own process issues, if they notice that
there's something wrong with staffing or this or that. But,
at a higher level, if they notice that a particular part of the Netherlands has
more stillbirths, then they look at it. So there's a local level of
accountability as well. They also have a higher doctor-patient ratio than other
countries. That's been constant over the time, but the progressive improvement
that they've demonstrated is incredible. It's very impressive.[82]
4.85
The mortality review process used in the Netherlands has two steps. The
first is a quick investigation to detect major patient safety or service
issues, often in the form of a root cause analysis. The second step involves a
more formal investigation between four and six weeks after the stillbirth and a
formal perinatal mortality review meeting at which the case is discussed.
Finally, the investigator meets with the bereaved family and outlines the
review outcomes. Parents may also attend the review meeting.[83]
...they took the aeroplane crash approach, which was to look at
the systemic errors all the way along. What they found was that talking to the
family within 48 hours of the loss to specifically identify what the parents'
questions were meant that, when the case was investigated, those questions
could be answered. So the parents were engaged in the process in a way where
every question they asked, whether it was important or not, was given an
answer. These are often given in a written document. The family is then engaged
again at the four-week point. They would speak to the families and do all of
the appropriate bereavement care again at that stage and make sure that they
were utilising the appropriate resources. Again, they would find out what the
family wanted to know et cetera.[84]
4.86
The Netherlands program also provided the basis for a successful
Scottish education program, Maternity Care Quality Improvement Collaborative,
implemented in 2011 and subsequently adopted in the UK (see Chapter 7).[85]
Autopsies and other post-mortem investigations
4.87
As noted above, PSANZ and Stillbirth CRE have developed a Clinical
Practice Guideline to improve maternity and newborn care for bereaved parents
and families, and to improve the quality of data on causes of stillbirth and
neonatal deaths through appropriate investigation, including autopsy, audit and
classification.[86]
4.88
The Guideline recommends that all parents be offered the option of a
high quality autopsy following stillbirth or neonatal death. Stillbirth CRE
considers autopsy to be the 'gold standard investigation' for perinatal deaths
and should be offered to parents by trained health care professional.[87]
4.89
The Guideline also recommends that, in the case of a stillbirth,
neonatal death or birth of a high risk infant, the placenta, membranes and cord
should be sent for examination by a perinatal/paediatric pathologist regardless
of whether consent for an autopsy has been granted.[88]
Low autopsy rates
4.90
Autopsy rates for perinatal death are low in Australia, despite advocacy
over a long period for more autopsies to be performed and particularly where a
cause of stillbirth has not been identified.[89]
4.91
Autopsy is not a mandatory reporting item in state and territory
perinatal data collections, and performance of an autopsy is not obligatory for
stillbirths unless the death is referred to a coroner. The rates of autopsy
therefore vary considerably across the states and territories, from 31 per cent
in Queensland to 62 per cent in WA. The autopsy rates are even lower for Aboriginal
and Torres Strait Islander stillbirths.[90]
4.92
In 2011−12,
for example, autopsies were conducted in 42.3 per cent of stillbirths in
Victoria, Queensland, WA, SA, Tasmania and the Australian Capital Territory.[91]
4.93
According to Stillbirth CRE, autopsy rates are higher and unexplained
stillbirth rates are lower in WA and SA, which may be explained by the
existence of coordinated perinatal services in those jurisdictions.[92]
4.94
Whilst the Clinical Practice Guideline has been in place for more than
10 years, it is not mandated.[93]
Between 2004 and 2008 the number of unexplained antepartum deaths was 1949, but
autopsies were undertaken for less than half of these (47 per cent). In
addition, whilst 40 per cent of babies may have some type of post-mortem
examination, only 20 per cent are given a full autopsy.[94]
4.95
The AIHW reported that in 2013-14 full autopsies were performed in only
21 per cent of stillbirth cases in Australia compared to the UK (43.5 per cent)
and New Zealand (42.5 per cent).[95]
4.96
Research into the low rates of autopsy in perinatal death cases suggests
that contributing factors include lengthy delays in finalising an autopsy, and
poor counselling of parents about the option of having an autopsy performed.[96]
Mr Haldane reported, for example, that he and his partner were told that a full
autopsy report may take 18 months to be completed.[97]
4.97
The length of time taken to complete an autopsy varies from state to
state. In Victoria, the Victorian Perinatal Autopsy Service (VPAS) completes
perinatal autopsies within eight weeks, as Associate Professor Kerryn Ireland-Jenkin,
Head of Unit at VPAS, explained:
Within two business days of a perinatal autopsy being done,
there should be what's called a preliminary report that goes back. The
preliminary report doesn't really provide a lot of pathology data, but it
basically says—this is important, because we have a service where people are
referring to three hospitals in Victoria: 'Your baby came to hospital X. An
autopsy was performed by Dr Y on this date. This is the list of investigations
that we performed in that autopsy. We will be issuing a final report within
eight weeks.' That fits with the requirement by NPAAC guidelines around autopsy
turnaround time. Why do we say eight weeks? Could we turn them around a little
quicker? It's often the ancillary investigations that take almost up to the
eight weeks—maybe the genetics, sometimes radiology et cetera. We feel that, if
we list that turnaround time, that's something that we think is absolutely
achievable, and we'd rather say something that's realistic and fits within
national guidelines than pretend we're offering something that is better than
we can actually offer, and then people are disappointed and make appointments
without data being available.[98]
4.98
In contrast, in NSW, an autopsy report can take more than 12 months to
be completed, forcing parents to wait for the information that may help them to
avoid a future stillbirth or other pregnancy complications.[99]
Queensland has been up to 18 months behind in its reporting, due to a lack of
resources and funding.[100]
4.99
Stillbirth CRE noted that lengthy waiting times and uncertainty around
timeframes for the results of autopsies and other investigations are a source
of distress for many bereaved parents.[101]
4.100
Dr Adrienne Gordon, Neonatal and Perinatal Medicine Specialist, Royal
Australasian College of Physicians (RACP), noted that there are less invasive
options available to families who do not wish to have a full autopsy conducted
on their baby.
You can have a post-mortem MRI scan and you can request just
an external examination of the baby by a skilled perinatal pathologist.
Obviously, the placenta is key, so it's very important that, if a family do
decline to have further examination with an autopsy, the placenta is still
looked at. I do think there are other options.[102]
4.101
Professor Jane Dahlstrom stated that examination of the placenta is an
important part of stillbirth investigation and influences the quality of the
data available. Professor Dahlstrom also considered that such investigations
should be undertaken by specialist perinatal pathologists, noting that: 'perinatal/placental
pathologists are more likely to detect significant disease in a placenta
associated with stillbirth than a general anatomical pathologist'.[103]
Associate Professor Ireland-Jenkin simply stated:
There are some of us who work in this area who feel that, if
we—this is pathologists—were only allowed to do one test in the investigation
of stillbirth and if you said to me, 'Would you like to examine the placenta or
would you like to perform the autopsy?' I think I would choose the placental
pathology, because I think it's incredibly important.[104]
4.102
There is, however, a lack of funding to undertake stillborn autopsies in
some jurisdictions, and this is compounded by a shortage of skilled
pathologists available to undertake autopsies on stillborn babies—an issue for high-income
countries more generally.[105]
4.103
Dr Gordon noted that, in NSW where the autopsy rate is relatively low,
the government has introduced a statewide perinatal pathology service that is
available to all families, regardless of their geographical location. The
service includes a coordinator and a central telephone number: 'It's all quite
new. But I guess one solution to limited numbers of people is having some
investment from the jurisdiction and a statewide service'.[106]
4.104
Similarly, the Victorian government has introduced a coordinated perinatal
autopsy service in public hospitals.[107]
The VPAS stated that the perinatal autopsy rate in Victoria is approximately 40
per cent, although it considered the optimal rate to be 60 per cent, and considered
that a centralised service was essential to achieving consistency in stillbirth
reporting and improvements in a hospital's procedures.
The value of a high quality, centralised perinatal
post-mortem service is that it provides high quality, consistent data regarding
the findings (report) in a case of perinatal death...A high quality perinatal
autopsy service reduces the rate at which cases of stillbirth are classified as
Unexplained, which is an important outcome.[108]
Autopsy costs and access
4.105
The committee heard that, since there is no funding available under the MBS
to undertake a stillbirth autopsy, the costs must be met by state/territory
health departments, hospitals or families.[109]
4.106
Associate Professor Ireland-Jenkin advised that the rebate levels for
autopsy in Victoria are set by, and the costs allocated to, the state
Department of Health and Human Services. She also explained:
There's no uniform rate of reimbursement across Australia. In
some healthcare jurisdictions, the number that's been quoted to me—and I don't
know the precise details—may be significantly higher than the current rates
that are set in Victoria. We did engage in creating a business case when the
service was set up at the start of 2016, when we looked at the number of hours
of pathologist time, registrar time et cetera. We did a really robust business
case.[110]
4.107
Other witnesses suggested that the cost of a perinatal autopsy is
between $3000 and $5000, but Professor Flenady explained that '[m]ost parents,
obviously, aren't charged. Even in the private system it will be absorbed.'[111]
Dr Diane Payton, Chair, Paediatric Advisory Committee, Royal College of Pathologists
of Australasia (RCPA) also discussed costs associated with transporting a baby
from a regional or remote location to a major metropolitan hospital so that an
autopsy can be performed.[112]
4.108
Research in other high-income countries identified similar problems,
with resources being diverted away from stillbirth investigations.
Failure to offer autopsy denies parents a chance to
understand the cause of their baby’s death, increases the proportion of
unexplained stillbirths, and hinders the effectiveness of subsequent audits. A
crucial shortage of perinatal pathologists also hampers efforts. Such a
shortage was shown in our surveys, where only 26% of care providers reported
that autopsies were undertaken or supervised by perinatal or paediatric
pathologists. Resources continue to be diverted away from perinatal pathology
services, despite stillbirths and neonatal deaths outnumbering all deaths from
cancer.[113]
4.109
Mrs Iverach stated that the available data for research is limited
because families are not being given sufficient support following a stillbirth,
resulting in the investigations of their baby's death not being completed.
The specialist reported to me that deaths are often listed as
“cord accident” and this does not give an accurate cause or indication of
factors involved...making this conclusion unhelpful in prevention or change. The
specialist stated that “cord accident” is often used when no other data is
available to make a full determination and this is the best conclusion they can
make.[114]
4.110
Dr Warland recommended supplementing clinical data collection by
introducing a standardised verbal autopsy from parents as soon as possible
after the stillbirth.
This verbal autopsy should include questions about whether or
not the mother noticed changes in her body and/or her unborn baby’s behaviour
in the days leading up to the stillbirth, what she did or didn’t do about it
and also what her maternity care provider did, or didn’t do, about it.[115]
Coronial investigations
4.111
Traditionally, Australian coroners have jurisdiction to investigate the death
'of persons who at some stage have been alive after they have been born'.[116]
The committee heard evidence from several witnesses about the merits of
extending coronial jurisdiction to cases of stillbirth.
4.112
Dr Warland noted that babies are not legal entities until they are born
live, and therefore stillbirths fall outside of the jurisdiction of coroners.
She argued that this is an anomaly that should be corrected, so that there is
greater accountability for stillbirth deaths.[117]
4.113
Some researchers have argued that coronial inquests are not the most
appropriate way of investigating stillbirths, and that autopsy and/or clinical
audits would be preferred options, with the responsible health care service
undertaking the audit, which would be reviewed by an independent external
panel.[118]
4.114
The UK is currently considering widening its coronial jurisdiction to
include certain cases of stillbirth, which is currently excluded on the basis
that there has to have been an independent life prior to coronial
investigation.[119]
4.115
In Australia, coroners do not investigate stillbirth, as 'a coroner has
jurisdiction not in respect of injuries or stillbirths but in respect of the
deaths of persons who at some stage have been alive after they have been born'.[120]
4.116
Mrs Dimitra Dubrow, Principal and Head of Medical Negligence, Maurice
Blackburn Lawyers, noted that coronial findings often drive reforms in
policies, procedures and standards, including increased awareness and
management of risks, the need for ongoing training for locum obstetricians and
a review of hospital procedures. She also noted that autopsy reports often
contain statements that are unhelpful and arbitrary, and that a coronial
investigation might yield significant new information about the circumstances
of stillbirth. She argued that a similar reform in Australia would ensure a
greater degree of independence, accountability and transparency in the process
of determining why unexpected stillbirths occur. She noted that a coronial
investigation should be used to determine the cause of stillbirth, rather than
being a 'fault-finding exercise'.[121]
4.117
Dr Carrington Shepherd, Co-Lead, Western Australian Perinatal
Epidemiology Group, considered that there is a need for a more systematic and
independent approach to port-mortem investigations of stillbirths. He proposed
that the National Coronial Information System, that includes information on
perinatal loss, could be expanded to include stillbirth and autopsy findings.[122]
4.118
Mrs Claire Foord, Chief Executive Officer and Founder of Still Aware, noted
that there is generally a gap in autopsy reports where no cause of death could
be determined, and called for the use of a coronial investigation in such cases
to ensure that all the available evidence from both clinical and family
perspectives is recorded and reviewed. Such an investigation would contribute
to a better understanding of the circumstances surrounding the stillbirth.
There are gaping holes in autopsy reports that say 'there was
no reason for anything to go wrong' or 'we have no understanding of any
precursor to this'. But the fact is they're not going to know that unless they
can go back and look at historical records and talk to all of the people
involved in this child's life, and that's parents included. So, we're asking
for the coroner to have jurisdiction not over every childhood death to
stillbirth but rather those that are preventable deaths in the third trimester
that can be reported, and as such it would be said, 'Okay the coroner should
have jurisdiction over this.'[123]
4.119
The National Perinatal Mortality Data Reporting Project noted that a
requirement for a coronial investigation can delay jurisdictions submitting
registration data to the ABS for inclusion in the national perinatal data
collections.[124]
Committee view
4.120
The lack of a consistent and coordinated approach to stillbirth at a
national policy level has contributed to a fragmentation of stillbirth
reporting and data collection, and is inhibiting efforts to undertake research
that will assist in reducing the incidence of stillbirth in Australia.
4.121
The committee heard evidence from leading stillbirth research
organisations that current national practice for stillbirth data collection in
Australia is 'suboptimal', and is significantly impacting on their ability to
answer important questions about the causes and prevention of stillbirth.
Contributing factors include duplication of effort and disparate approaches
across and within states and territories; fragmented data collections that do
not link maternal health, pregnancy and birth risk factors; and a system that
is fraught with delay and unresponsive to change.
4.122
The lack of progress in reducing stillbirth rates in Australia
highlights the urgent need for a multi-jurisdictional commitment to systematic
stillbirth reporting and data collection. This is crucial if governments are to
provide researchers with reliable, timely and consistent data at a granular
level necessary for the development of targeted, evidence-based prevention
strategies.
4.123
The committee acknowledges the Australian government's proposed data
sharing and release legislation that aims to enhance the integrity of the
public sector data system and make it more accessible to researchers.[125]
It urges the government to take into consideration, as part of its
consultation, the need for Australian stillbirth researchers to have access to a
NPMDC that is high-quality, timely, consistent, detailed, and cost-effective to
access. It notes that the Vital Statistics Online Data Portal in the USA offers
a best practice model that, if adopted in Australia, would ensure that
stillbirth researchers are no longer hampered in their efforts to reduce the
unacceptably high rate of stillbirth in Australia.
4.124
The committee also acknowledges the importance of the current PHRN-led
project, being undertaken as part of the National Collaborative Research
Strategy, which aims to improve linkages between state/territory data
collections and the national data collections through the AIHW.
4.125
Whilst such initiatives are welcome, the paucity of timely, high-quality
data on stillbirth remains a significant impediment to determining national
research priorities, addressing substandard care, identifying causes and risk
factors, and establishing evidence-based prevention strategies.
Recommendation 2
4.126
The committee recommends that the Australian Health Ministers' Advisory
Council agrees to prioritise the development of a comprehensive, standardised,
national perinatal mortality data collection that:
- includes information on timing and cause of death, autopsy and
termination of pregnancy; and
-
links to the National Death Index and perinatal mortality data
collections to utilise information on maternal health, pregnancy and birth risk
factors.
4.127
The committee urges the AHMAC to consider endorsing the strategies
proposed by the Stillbirth CRE, as follows:
- adopting a single national definition for stillbirth to be used
by all jurisdictions;
-
implementing a standardised national electronic reporting system
to collect 'real-time' data on births and deaths, including identification of Aboriginal
and Torres Strait Islander and other high risk groups;
-
including stillbirth rates as key performance indicators in
annual perinatal outcomes reports; and
-
undertaking hospital level audits to identify contributing
factors relating to care in relation to stillbirths and neonatal deaths.
4.128
Determining the cause of a baby's death is one of the most significant questions
surrounding stillbirth, and the lessons learned from reviews of medical data
are important for improving research and education as well as clinical
practice. Successful international programs such as MBRRACE-UK offer valuable
models for a more collaborative, multi-jurisdictional approach to perinatal
mortality review programs. However, the committee heard that the number of
perinatal mortality audits in Australia is low and represents a significant
barrier to reducing the rate of stillbirths in Australia.
4.129
The committee notes that there is no funding available under the MBS to
undertake a stillbirth autopsy, and that the costs must be borne by
state/territory health departments, hospitals or families. According to state
and territory agencies responsible for data collection, it can take several
years to implement a new mandatory reporting item.
4.130
The lack of funding is contributing to delays in the results being made
available to bereaved parents as well as to researchers. In addition, the
current process for extending MBS funding requires review in order make it
sufficiently flexible to accommodate breakthroughs in medical research and
technology (see, for example, the discussion on genetic testing in Chapter 5).
Recommendation 3
4.131
The committee recommends that the Australian government seeks advice
from the Medical Services Advisory Committee on the economic costs and benefits
of adding stillbirth autopsies as a new item in the Medicare Benefits Schedule,
and urges the government to consider funding the projected cost of this new
item in the 2019−20
Federal Budget.
4.132
The committee acknowledges that Australia has a critical shortage of
perinatal pathologists, severely restricting the number of autopsies and other
pathology services being conducted following stillbirth. Unless more resources
are provided for training and employing perinatal pathologists, efforts to
reduce the rate of stillbirth will continue to be hampered by insufficient
information and data about the causes of stillbirth. This shortage of skilled
perinatal pathologists has significant implications for bereaved parents,
clinicians, health professionals and researchers seeking to understand and
address the causes of stillbirth.
Recommendation 4
4.133
The committee recommends that the Australian government consults with
the Royal College of Pathologists of Australasia and relevant education and
training authorities to identify strategies for increasing the number of
perinatal pathologists available to undertake stillbirth investigations in
Australia, including identifying costs and sources of funding.
Navigation: Previous Page | Contents | Next Page