Overview of crystal methamphetamine and its use in Australia
2.1
This chapter provides a summary of crystal methamphetamine and its use
in Australia. It first defines crystal methamphetamine and how it differs from
other methamphetamine substances; it then explores the following matters:
-
Crystal methamphetamine use in Australia, the number of users and
the difficulty estimating the quantity of crystal methamphetamine consumed each
year.
-
Problematic versus non-problematic use and the identification of groups
at risk of developing problematic consumption behaviours.
-
The mental and physical effects of crystal methamphetamine,
specifically methamphetamine-induced psychosis and violent behaviours demonstrated
by some users.
-
Drivers of crystal methamphetamine use and factors that contribute
to problematic use.
-
Price, purity and methods of administration.
-
Poly-drug use as a feature of crystal methamphetamine use and how
this influences users' health outcomes.
-
National data on illicit drug arrests and illicit drug offences
recorded in the criminal courts of each state and territory.
What is crystal methamphetamine?
2.2
Crystal methamphetamine is a form of methamphetamine,[1]
grouped under the class of amphetamine-type stimulants (ATS). The term
'crystal' refers to its crystalline structure, which gives the substance the
appearance of crushed ice,[2]
hence its colloquial name of 'ice'.
2.3
Various common or street names for methamphetamines with reference to
their forms and methods of administration are outlined in Table 1.
Table 1: common names for methamphetamines[3]
| Drug type |
Common names |
Forms |
Method of
administration |
| Methamphetamine |
Meth, speed, whiz, fast,
uppers, goey, louee, Lou Reed, rabbit, tail, pep pills.
In paste form it can be
referred to as base, pure or wax.
In liquid form it can be
referred to as ox blood, leopard's blood, red speed or liquid red. |
White, yellow or brown
powder, paste, tablets or a red liquid |
Oral, intranasal,
injection, anal. |
| Crystal methamphetamine |
Ice, dmeth, glass,
crystal, batu, shabu (in South-East Asia) |
Crystalline |
Smoking, intranasal,
injection |
2.4
Some evidence presented in this report refers to crystal methamphetamine
specifically, while other evidence describes methamphetamine and/or amphetamine.
Generally, methamphetamine is referred to when specific data on crystal
methamphetamine is not available. Australia's federal law enforcement agencies
refer to methamphetamine as methylamphetamine.
2.5
During the course of the inquiry, many witnesses rejected the term 'ice'
on the basis this term can have positive connotations and potentially encourage
use. For this reason, this report refers to crystal methamphetamine,
methamphetamine or amphetamine, as appropriate, unless directly quoting
evidence where another name for the drug was used.
Crystal methamphetamine use in Australia
2.6
Accurately ascertaining crystal methamphetamine use in Australia is
difficult, as it is for all illicit substances, due to a paucity of data and
limitations on the accuracy of the data that is available. Despite this,
Australia has a number of initiatives and longitudinal studies that provide
authorities and those working in the alcohol and other drug (AOD) sector with some
insight into the consumption of illicit substances. These include:
-
the National Drug Strategy Household Survey (household survey);
-
the Drug Use Monitoring in Australia (DUMA) program;
-
the Illicit Drug Reporting System (IDRS);
-
Clients of Alcohol and Other Drug Treatment Service (AODTS); and
-
the recently established National Wastewater Drug Monitoring
Program.
2.7
These initiatives are discussed in detail below.
National Drug Strategy Household
Survey
2.8
Every three years the Australian Institute of Health and Welfare (AIHW)
conducts the household survey and reports on alcohol, tobacco and illicit drug
use in Australia. The survey includes data on people's attitudes and
perceptions about alcohol, tobacco and illicit drug use. The survey allows the AIHW
to collect data from nearly 24 000 people[4]
across Australia, mostly aged 14 years or older.[5]
Key findings from the 2016 National
Drug Strategy Household Survey[6]
2.9
The 2016 household survey showed a decline in recent self-declared use
(defined as use of an illicit drug in the last twelve months) of
meth/amphetamine from 2.1 per cent in 2013 to 1.4 per cent in 2016. Data
from the household survey indicates that the percentage of people using
meth/amphetamine has continued to decline since 2001 (see Table 2).
Table 2: Meth/amphetamine drug use,
people aged 14 years or older, 1993 to 2016[7]
| Year |
1993 |
1995 |
1998 |
2001 |
2004 |
2007 |
2010 |
2013 |
2016[8] |
| Meth/amphetamine[9]
(per cent) |
2.0 |
2.1 |
3.7 |
3.4 |
3.2 |
2.3 |
2.1 |
2.1 |
1.4 |
2.10
Despite the overall decline, the 2016 survey demonstrated that crystal
methamphetamine remains the preferred form of meth/amphetamine for users:
57 per cent of recent users reported that crystal methamphetamine is
their main form of meth/amphetamine used in the previous 12 months (an
increase of 7 per cent compared to 2013).[10]
This result continues an upward trend observed since 2010 (see Table 3).
Table 3: Main form of
meth/amphetamine used in last 12 months, people aged 14 years or older, 2007 to
2016[11]
| Drug |
2007 |
2010 |
2013 |
2016 |
| Powder/Speed |
51.2 |
50.6 |
28.5 |
20.2 |
| Crystal/ice |
26.7 |
21.7 |
50.4 |
57.3 |
| Base/paste/pure |
12.4 |
11.8 |
7.6 |
1.6 |
| Tablet |
5.1 |
8.2 |
8.0 |
5.6 |
| Prescription
amphetamines |
3.2 |
6.8 |
3.0 |
11.1 |
| Liquid |
1.3 |
0.9 |
0.5 |
n.p |
| Capsules |
NA |
NA |
2.0 |
3.8 |
2.11
The 2016 survey also reported that the frequency of meth/amphetamine
use has increased, in particular for those people using crystal methamphetamine
(see Tables 4 and 5).
Table 4: Frequency of
meth/amphetamine use by recent users aged 14 years or older (all recent
meth/amphetamine users)[12]
| Frequency of use |
2007 |
2010 |
2013 |
2016 |
| At least once a week or more |
13.0 |
9.3 |
15.5 |
20.4 |
| About once a month |
23.3 |
15.6 |
16.6 |
10.6 |
| Every few months |
27.9 |
26.3 |
19.8 |
24.7 |
| Once or twice a year |
35.6 |
48.8 |
48.0 |
44.3 |
Table 5: Frequency of
meth/amphetamine use by recent users aged 14 years or older (frequency of
crystal methamphetamine use)[13]
| Frequency of use |
2007 |
2010 |
2013 |
2016 |
| At least once a week or more |
23.1 |
12.4 |
25.3 |
31.9 |
| About once a month |
24.3 |
17.5 |
20.2 |
8.3 |
| Every few months |
20.7 |
23.1 |
14.3 |
22.6 |
| Once or twice a year |
31.8 |
47.0 |
40.2 |
37.3 |
Perceptions and attitudes towards
meth/amphetamine
2.12
The household survey also surveys respondents' perceptions and attitudes
towards illicit drugs. Despite the overall decline in use, the perception that
meth/amphetamines are causing social and criminal problems has increased.
2.13
Household survey data shows a significant increase in the number of
people who believe that meth/amphetamines are the most concerning drugs for the
general community and in 2016, for the first time, meth/amphetamines overtook
the excessive consumption of alcohol as the drugs of most concern (see Table 6).
Meth/amphetamines were also considered the drugs most likely to be associated
with a 'drug problem' (21.9 per cent in 2013 to 46.4 per cent in 2016).[14]
Table 6: Drug thought to be of most
concern for the general community, people aged 14 years or older, 2007 to 2016[15]
| Drug |
2007 |
2010 |
2013 |
2016 |
| Excessive drinking of alcohol |
32.3 |
42.1 |
42.5 |
28.4 |
| Cannabis |
5.7 |
4.5 |
3.8 |
2.6 |
| Meth/amphetamine |
16.4 |
9.4 |
16.1 |
39.8 |
| Cocaine |
8.3 |
6.1 |
3.6 |
3.3 |
| Ecstasy |
6.0 |
5.5 |
5.2 |
5.0 |
| Heroin |
10.5 |
11.4 |
10.7 |
7.5 |
2.14
The 2016 household survey noted that factors, such as media coverage and
personal experiences, are likely to influence the opinions of respondents in
terms of perceptions of and attitudes towards illicit drugs.[16]
2.15
The committee heard evidence from Professor Rebecca McKetin in 2015 and
again in 2017. Professor McKetin referenced a detailed study of the household
survey conducted by Professor Anne Roche. This study showed that prevalence of
use was stable but this was not consistent across regions. It found use in
regional areas had increased, whilst it had decreased in metropolitan areas.
Professor McKetin said researchers have followed these indicators and:
...there is certainly a broad range of indicators consistently
showing an increase. There is definitely an increase in the level of
problematic use and there is a little evidence of an increase in the uptake of
use too, but I think it is important to understand that the situation is not
the same everywhere, so you cannot make one sweeping statement that things have
not changed.[17]
2.16
Professor McKetin also explained that the study of the household survey
shows evidence that there has been under-reporting of methamphetamine use,
which she believes may explain for the disparate trends in other indicators and
the survey.[18]
Professor Steve Allsop from the National Drug Research Institute (NDRI) added
that:
We also have to recognise that, for all sorts of reasons, we
end up with underreporting. There is a high nonresponse rate. Many of the
people who might be particularly at risk are more likely to be non-respondents;
for example, people who are in the prison system, people who do not have phones
or addresses that are easily contactable, people who choose not to respond—or
to not respond accurately—or sometimes people do not even know accurately. For
example, if you ask people how much alcohol they have consumed, some people
underreport deliberately and some people do not have a good idea.[19]
2.17
This issue had been raised by Professor McKetin in earlier evidence
provided to the committee:
There is also an issue with population surveys that they
quite strongly underrepresent problematic drug use, and they are very sensitive
to any stigma around drug use. There is negative publicity, and we have seen
this before for methamphetamine; you get strong underreporting. If you look
back to the 2001 survey, almost 10 per cent of Australians said they had ever
used speed, amphetamine and methamphetamine. By 2007, after all of the bad
press, that fell to 6 per cent. Suddenly 4 per cent of Australians who had used
methamphetamine no longer have used methamphetamine. That is the extent of
underreporting that you can get.[20]
2.18
The Department of Health addressed the issue of under-reporting in the
household survey. It acknowledged that having people admit to an illegal
activity may lead to under-reporting, but:
That is the way people answer, and there is nothing you can
do to control that. However, I would point to, if there is underreporting—and I
do not know whether there is—you can still look at the trends in the data. You
would assume that you would be getting the same kind of underreporting or
over-reporting or whatever it might be. The way statisticians work with data is
to work out what the degrees of error are.[21]
Drug Use Monitoring in Australia
program
2.19
The DUMA program measures drug use amongst police detainees from nine
sites across Australia. This ongoing study examines the relationship between
drugs and crime, local drug markets and patterns of use by detainees. DUMA data
is collected and published periodically by the Australian Institute of
Criminology (AIC). Its last publication was on 9 February 2016, as a part of a
series of papers about methamphetamine use and the perspectives of DUMA police
detainees.[22]
The Drug use monitoring in Australia: 2013–14 report on drug use among
police detainees is the last full year analysis publicly available on the
AIC website, but the Australian Criminal Intelligence Commission's (ACIC) Illicit
Drug Data Report 2015–16 notes results from the 2014–15 and 2015–16 DUMA
examinations.
2.20
According to the Illicit Drug Data Report 2015–16, the number of
detainees testing positive for amphetamine use increased, from 40.9 per cent in
2014–15 to 50.5 per cent in 2015–16. This recent result marked the
'highest percentage reported in the last decade'.[23]
The ACIC identified the increase in detections of methamphetamine
(methylamphetamine) use in detainees as the reason for the continued upward
trend in detections, with data showing an increase from 38.7 per cent in
2014–15 to 49 per cent in 2015–16. Further:
The proportion of detainees testing positive for
methylamphetamine continues to be higher than the proportion testing positive
for MDMA,[24]
heroin, cocaine, benzodiazepines and opiates (excluding heroin). In 2015–16,
the proportion of detainees testing positive for methylamphetamine was higher
than the proportion testing positive for cannabis (44.4 per cent). In 2015–16,
59.7 per cent of detainees self-reported recent methylamphetamine use, an
increase from the 50.4 per cent reported in 2014–15.[25]
Illicit Drug Reporting System
2.21
Since 1999, the IDRS has monitored illicit drug use across all states
and territories. The IDRS provides a coordinated monitoring system with a
particular focus on heroin, methamphetamine, cocaine and cannabis. The IDRS comprises
interviews with people who inject drugs, interviews with experts, and the
examination of other data sources, such as opioid overdose data, treatment
data, and purity of seizures of illicit drugs made by law enforcement agencies.[26]
2.22
Key findings from the IDRS for 2016 showed:
-
75 per cent of the national sample reported 'using one or more
forms of methamphetamine in the last six months on a median of 36.5 days',
significantly higher than the 2015 median of 24 days;[27]
-
recent use of crystal methamphetamine was significantly higher,
with use increasing from 67 per cent in 2015 to 73 per cent in 2016;
-
the frequency of use in the last six months for crystal
methamphetamine had increased from 20 days in 2015 to 30 days in 2016 in total;
and
-
the majority of methamphetamine users administered the drug
through injections; and this method was common to all forms of methamphetamine
(see Table 7).[28]
Table 7: Proportion of people who
inject drugs that reported use of crystal methamphetamine in the preceding six
months, by jurisdiction, 2010–2016[29]
| % |
National |
NSW |
ACT |
Vic. |
Tas. |
SA |
WA |
NT |
Qld. |
| 2010 |
39 |
48 |
48 |
36 |
20 |
60 |
40 |
18 |
37 |
| 2011 |
45 |
53 |
57 |
53 |
26 |
44 |
46 |
28 |
50 |
| 2012 |
54 |
68 |
66 |
59 |
43 |
56 |
64 |
26 |
44 |
| 2013 |
55 |
74 |
61 |
55 |
45 |
57 |
59 |
30 |
50 |
| 2014 |
61 |
74 |
72 |
75 |
54 |
60 |
53 |
26 |
58 |
| 2015 |
67 |
65 |
79 |
71 |
59 |
70 |
64 |
60 |
62 |
| 2016 |
73 |
77 |
78 |
73 |
73 |
75 |
62 |
69 |
69 |
Clients of Alcohol and Other Drug
Treatment Services
2.23
The AIHW collects data as part of the Alcohol and Other Drug Treatment
Services National Minimum Data Set (AODTS NMDS). Data included in the AODTS
NMDS is from treatment provided by publicly-funded AOD treatment agencies in
Australia. Since 2003–04, the AIHW releases the Clients of AODTS reports.[30]
2.24
The Clients of AODTS report for 2015–16 found that 23 per cent of
closed treatment episodes[31]
had amphetamines listed as the principal or additional drug of concern.[32]
There were 46 441 treatment episodes for amphetamines in 2015–16, an increase[33]
from 32 407 treatment episodes in 2014–15 (see Table 8).[34]
Table 8: National closed treatment
episodes for clients own drug use by principal drug of concern, 2010–2016[35]
| Year |
2010–11 |
2011–12 |
2012–13 |
2013–14 |
2014–15 |
2015–16 |
| Amphetamine |
12 563 |
16 875 |
22 265 |
28 919 |
32 407 |
46 441 |
National Wastewater Drug Monitoring
Program
2.25
On 26 March 2017, the ACIC released its first report from the National
Wastewater Drug Monitoring Program (wastewater program's first report). The
wastewater program was established in June 2016 after $3.6 million was
allocated from the Confiscated Assets Fund to fund it.[36]
The wastewater program tests for 13 drugs, both illicit[37]
and licit.[38]
The data collected captures approximately 14 million Australians (58 per
cent of the population).[39]
2.26
The wastewater program's first report argued that methamphetamine 'is
the highest consumed illicit drug tested across all regions[40]
in Australia'.[41]
Although the wastewater analysis has found methamphetamine use to be high, the exclusion
of cannabis (THC)[42]
has meant this finding conflicts with some other evidence. For example, the 2013 household
survey showed the most common illicit drug used both recently and over participants'
lifetime was cannabis, 'used by 10.2 per cent and 35 per cent respectively of
people aged 14 and over'.[43]
2.27
The wastewater program's first report noted:
-
the capital city sites in Tasmania and the Australian Capital
Territory showed the lowest levels of methamphetamine in their wastewater;
-
methamphetamine detections in South Australian (SA) city sites
exceeded detections in SA regional sites;
-
methamphetamine detections in wastewater over the past five years
at the Queensland and SA sites have shown a consistent pattern of increasing
levels;[44]
-
Western Australia (WA) has the highest levels of methamphetamine
in its wastewater, with detection in both city sites and regional sites far
exceeding the national average;
-
several regional sites in Queensland, Victoria and Tasmania show
high levels of methamphetamine detection; and
-
Australia ranks second out of 18 countries for consumption of
methamphetamine (Slovakia is ranked first).[45]
2.28
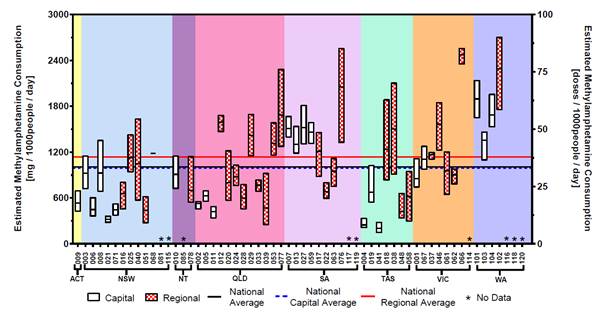
Figure 1 is extracted from the wastewater program's first report. It
shows the estimated amount of methamphetamine consumption per thousand people
and doses per day at each of the testing sites. Data is separated by state and
territory and by capital region and regional area. Finally, the figure
indicates both national capital average and regional average (the red and blue
lines). The figure shows regional consumption rates in WA, SA and Queensland
are far higher than the national regional average. Data from WA and SA show
above average consumption in capital areas.
Figure 1: Estimated methamphetamine
consumption in mass consumed per day (left axis) and doses per day (right axis)
per thousand people. The number of collection days varied from 1–7[46]
2.29
The national wastewater program compliments other wastewater analysis,
such as the University of South Australia's Drug use in Adelaide Monitored by Wastewater
Analysis reports (SA analysis), commissioned by the Drug and Alcohol Services
South Australia. This analysis commenced in 2011 and focuses on metropolitan
Adelaide. Unlike the national program, the SA wastewater analysis includes
heroin[47]
and cannabis.[48]
2.30
The SA analysis for April 2017 showed methamphetamine use in metropolitan
Adelaide slowly increasing between 2012 and December 2016. However, there has
been a steady decline during the reporting periods for 2017.[49]
2.31
On 27 July 2017, the ACIC released the wastewater program's second report.
This second wastewater report found that methamphetamine remained the highest
consumed illicit drug tested across all regions; however, nationally there has
been a slight reduction in methamphetamine detections when compared to the
first reporting period.[50]
Testing sites in the Northern Territory (NT) and Tasmania[51]
did not participate[52]
in the second reporting period.[53]
2.32
The second wastewater report found detections were highest in SA and WA.[54]
For both these states, use appears to have peaked in October 2016 and has
subsequently declined since. Queensland shows a similar pattern, although less
pronounced.[55]
The ACIC concluded that:
The overall picture for methylamphetamine is one of ongoing
and strong demand. While the National Wastewater Drug Monitoring Program has
shown signs that consumption may have peaked in late 2016, it is too early to
say with any certainty if this recent reduction in consumption is the start of
a longer term trend.[56]
Problematic versus non-problematic use
2.33
Despite the number of users and the negative effects of crystal
methamphetamine use, numerous submitters and witnesses advised the committee
that the majority of individuals who use the drug do not demonstrate problematic
use (such as anti-social or criminal behaviour) and live normal and productive
lives. Further, although crystal methamphetamine impacts on a wide range of
individuals from across Australia, there are particular communities and groups
that are more at risk of developing problematic crystal methamphetamine use.
2.34
The Australian Injecting and Illicit Drug Users League observed that a
small minority of people, approximately 15 per cent, use crystal
methamphetamine on a regular or daily basis. The remaining '85 per cent are
engaging in more irregular or occasional use, and perhaps less problematic use—that
is, less than weekly and, for most, less than monthly'.[57]
2.35
The Australian Federation of AIDS Organisations described the majority
of crystal methamphetamine users as non-problematic, that is:
...problematic in being contrary to criminal law but not
necessarily problematic in terms of health use. However, we do acknowledge that
for some people there are problematic levels of ice use...[it is] [n]ot
problematic in terms of being able to function.[58]
2.36
Dr Alex Wodak, President of the Australian Drug Law Reform Foundation
(ADLRF) commented on the differences between problematic and non-problematic use
of crystal methamphetamine. Referring to a series of longitudinal studies for
cocaine and amphetamine, Dr Wodak stated that people who consume 'impressive
quantities' of these drugs 'never came to the attention of law enforcement or
health services for their drug problem' and '[w]hen they started getting some
difficulties, they managed to work out how to pull themselves back'.[59]
Further, Dr Wodak argued that:
...although it does not seem to be something that we would leap
at believing, the evidence is fairly clear that some people are able to use
powerful psychoactive substances for long periods and monitor their own
behaviour to a surprising degree. That is not to say that that is recommended.
I do not recommend it and I am not calling for people to do that, clearly. I
spent the last 30 years dealing with people who got into serious trouble—some
died—caused great misery and anxiety to their families, caused great pain and
suffering in the community generally and were struggling with psychoactive drug
use. So I am not a fan of people getting into trouble with drugs, but we have
to acknowledge the truth, and the truth is: yes, some people can manage to
consume significant quantities of these drugs and somehow not get into trouble.[60]
...people who used large quantities of drugs and started to
have some difficulty pulled themselves up. They would say, 'I'm not going to
take any cocaine for three months,' or six months, or 'I'm only going to take
it on weekends,' or 'I'm not going to spend more than $30 a day on it.' They made
up some rule and stuck to it. After they got it under control, they would go
back. A lot of people monitor their own behaviour in other areas in a similar
way. We have to remember that a lot of people who have problems with
psychoactive drugs in the community do get better by themselves. There is a lot
of resilience in human beings.[61]
2.37
Although problematic crystal methamphetamine use may not eventuate for all
users, the Penington Institute highlighted that problematic use can adversely
affect 'people from all backgrounds and from all geographic areas' and:
...the spread of ice use in Australia has proven that drugs are
available in country areas—in regional and rural and even remote areas—just as
much as they are in the big cities. We have heard stories of the landed big
farming families—very well-to-do families—having problems with ice in their own
families, right down to the most socially disadvantaged and marginalised
communities. The people that get addicted and cause most of the problems
typically have pre-existing mental health issues like depression or anxiety,
and sometimes for those people ice is the first time they have ever experienced
great pleasure in their life. So they go back to it, and sooner rather than
later they are addicted.[62]
Young people
2.38
Evidence presented to the committee identified young people as being
more likely to use crystal methamphetamine and at greater risk of problematic
use. The household survey for 2013 showed that 41 per cent of people between
the ages of 20 and 29 years identified amphetamine as their principal drug of
concern[63]
when seeking treatment.[64]
Amphetamine was identified as an additional drug of concern for
36 per cent of people aged between 20 and 29 years who sought
treatment during the surveyed period.[65]
2.39
Professor Rebecca McKetin, at the time based at the Australian National
University, warned the committee that the uptake of crystal methamphetamine
amongst young people is an indicator of the beginning of an epidemic.[66]
Further, Professor McKetin advised that trends show there has been a 'doubling
of the number of heavy users' of crystal methamphetamine and the 'increase was
strongest in the under-24 age group'.[67]
Although heavy use had increased for people aged 24 or under, the bulk of users
are people in their 30s.[68]
2.40
The committee heard anecdotal evidence from staff involved in front line
treatment of problematic use that there has been an increase in the number of
young people seeking crystal methamphetamine treatment. A particular concern of
Queensland Health was the early age of people initiating the use of crystal
methamphetamine. Historically, those entering treatment programs were 17 or 18
years old, but Queensland Health staff expressed concern that they are now
seeing 15 and 16 year olds coming through their service.[69]
Kidz Youth Community Consultancy advised that it has provided treatment for
children as young as 10 and that adolescents and young people who are
experimenting with crystal methamphetamine are:
...unfortunately more inclined to become [dependent]. It is one
of the characteristics we are seeing with [crystal methamphetamine]. For our
service, probably about 40 per cent of the young people are staying on it quite
heavily, whereas others may binge use and then stop using for a little while
and then binge use, depending on availability and also on whether there are
other drugs around at the time.[70]
2.41
Research by Professor Louisa Degenhardt et al published in the Medical
Journal of Australia indicates that the number of dependent and regular
users of methamphetamine in Australia has increased since 2010, especially in
the 15–24 and 25–34 age groups. The research found:
Rapid uptake of methamphetamine use may still be occurring
outside the largest cities, especially in regional centres where young people
without prior experience of methamphetamine may be exposed to it. The available
data, together with findings reported in this article, suggest a sharp increase
in problematic methamphetamine use among particular subgroups (particularly
young people) in Australia.[71]
2.42
Other factors relating to the uptake of crystal methamphetamine among
young people include its availability and affordability (discussed further at
paragraph 2.105–2.107) and whether those using the drug are a member of one
of the vulnerable categories described in the following sections.
Regional and rural communities
2.43
The committee heard that regional and rural communities are particularly
vulnerable to problematic crystal methamphetamine use. According to the AIHW,
people living in remote and very remote regions 'were at least twice as likely
to have used meth/amphetamines in the previous 12 months as people living in
Major cities and Inner regional areas'.[72]
2.44
Table 9 outlines data provided by the AIHW demonstrating differences in
meth/amphetamine use between those located in major cities compared with those
in regional and remote areas.
Table 9: Meth/amphetamine use,
people aged 14 years or older, by remoteness area (2007 to 2013)[73]
|
|
Ex-users[74] |
Recent users[75] |
| Remoteness/Year |
2007 |
2010 |
2013 |
2007 |
2010 |
2013 |
| Major cities |
3.9 |
5.1 |
4.3 |
2.5 |
2.0 |
2.1 |
| Inner regional |
3.2 |
4.1 |
4.1 |
1.7 |
2.0 |
1.6 |
| Outer regional |
4.1 |
4.4 |
4.0 |
1.6 |
1.5 |
2.0 |
| Remote/very remote |
5.7 |
7.2 |
8.6 |
3.0 |
4.0[76] |
4.4[77] |
2.45
The ACIC's wastewater program similarly highlighted differences
in methamphetamine use between capital and regional sites across Australia. The
program's first report shows WA with the highest levels of methamphetamine, in
both capital and regional areas.[78]
Regional areas had higher levels of methamphetamine use compared to capital
sites, except for SA and the NT.[79]
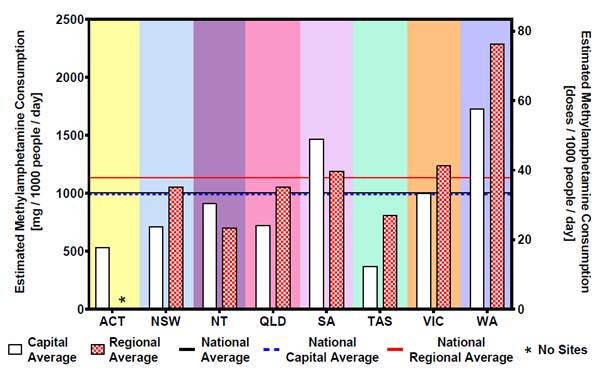
2.46
Figure 2 is extracted from the wastewater program's first report. It
shows the estimated amount of methamphetamine consumption per thousand people
and doses per day. Data is separated between capital and regional areas, and by
state and territory. The figure shows both the national capital average and
regional average. Regional consumption in SA, Victoria and WA is above the
national average. WA and SA have higher average consumption of methamphetamine
than other state and territories.
Figure 2: Estimated average
consumption of methamphetamine for capital city sites and regional sites by
state/territory[80]
2.47
According to the National Rural Health Alliance's Illicit Drug use in
Rural Australia report, the causes of illicit drug use in rural and remote
areas are multiple and inter-related: '[d]istance and isolation, poor or
non-existent public transport, a lack of confidence in the future and limited
leisure activities all contribute to illicit drug use in rural communities'.[81]
2.48
The unique challenges faced by regional and rural communities were raised
by a number of submitters and witnesses. Professor Ann Roche from
Flinders University observed that regional and rural communities are more
'likely to experience greater levels of consumption of alcohol and have associated
problems with alcohol' and that '[h]igher levels of most illicit substances
tend to concentrate where they have access to these drugs in regional and rural
areas'.[82]
The reason, according to Professor Roche, is that at a social level:
...where you have communities where there are higher levels of
unemployment and social disadvantage and higher levels of depression and mental
health problems, as you often get in many regional and rural communities, and
fewer life opportunities the individuals in those communities are more
vulnerable to the use of substances that are basically going to make them feel
better when life is not looking particularly good.[83]
2.49
She argued that this issue must be a major consideration for government
when forming appropriate response strategies to problematic drug use in those
communities.[84]
2.50
Another significant issue facing people in regional and rural areas is
accessing treatment services. According to the Victorian Alcohol and Drug
Association (VAADA), individuals from regional and rural communities have less
access to health services, including both primary health and AOD treatments.
Primary health care is limited in regional and rural areas with 3.6 general
practitioners available per 10 000 head of population, compared to 7.6 general
practitioners per 10 000 in metropolitan areas.[85]
Distance, privacy, availability, and simple staffing of services all create
barriers for those in rural communities to access AOD treatments.[86]
2.51
A further hurdle facing people from regional and rural communities, as
described by the Australian Psychological Society (APS), is that once users
return to the 'real world' after seeking treatment, they can find themselves
back in their community 'where everyone is using and [they] are not'. Those trying
to recover from addiction are:
...discharged back to [their] community where there is nothing.
[They] can go from seeing a counsellor every day or once a week in a very
supportive community to being discharged back to [a] community in some regional
place where [they] will get no access to any support at all.[87]
2.52
As discussed above, a number submitters and witnesses stated that people
from regional and rural communities are at a higher risk of developing
problematic crystal methamphetamine use. By contrast, others suggested that
this was not necessarily the case. For example, Drug Arm Australasia argued
that its data does not indicate a 'real difference in presentation rates'
between metropolitan and regional and remote areas. The problem was instead the
visibility of those people using crystal methamphetamine because 'in a metro
region you have the dilution effect that you do not have in a regional area'.[88]
2.53
Professor Paul Dietze, the Deputy Director of the Burnet Institute,
indirectly supported Drug Arm Australasia's comments. He informed the committee
that although there was sufficient anecdotal evidence describing the negative
effects of methamphetamine related problems in regional and remote communities:
...whenever we look closely at those reports, there is really
not much evidence to support them in terms of some of the indicator data that
are there. When I talk about indicator data, I mean things like ambulance
attendances and so forth.[89]
2.54
The problem, as detailed by Professor Dietze, is not necessarily that
there is no problem with crystal methamphetamine use in regional and rural
communities, but there is 'very little reasonable data from regional Australia'[90]
and for this reason:
We do not really have a good picture of what is going on...We
really have not made an investment in trying to find out what is actually going
on, either. We need to be moving beyond anecdote in relation to these parts of
the country.[91]
Indigenous communities
2.55
The committee heard that Australia's Indigenous communities are at a
higher risk of developing problematic crystal methamphetamine use. Indigenous
communities share the same vulnerabilities as other people found in regional
and remote communities;[92]
however, these vulnerabilities are more complex due to other factors such as the
'disparity in the general health of Aboriginal Australians compared to non-Indigenous
Australians'[93]
and the imprisonment rates of Indigenous people being '14 times higher than the
rate of non-Indigenous population'.[94]
The National Aboriginal & Torres Strait Islander Legal Service said that Indigenous
communities 'are at a higher risk of complex trauma because of the legacy of
colonisation, stolen generation policies, loss of land and ongoing racism and
discrimination which places them at greater risk of drug abuse'.[95]
2.56
The AIHW reported that 'Aboriginal and Torres Strait Islander people
were 1.5 times[96]
more likely to have recently used meth/amphetamine than non-Indigenous people'.[97]
However, Youth Off the Streets was concerned that research into Indigenous
communities and drug use has been primarily focused on Indigenous people in
urban areas and there is limited data on usage rates for Indigenous peoples in
regional and remote areas.[98]
According to a 2012–13 National Australian Aboriginal and Torres Strait
Islander Health Survey, 2.7 per cent of Indigenous Australians living in
non-remote areas reported the use of speed or amphetamine in the past year.[99]
2.57
The NT Police told the committee that there are a small number of known Indigenous
meth/amphetamine users in the NT and that these users are largely from urban
centres. The NT police also advised that there is use in some remote
communities[100]
but that it is not widespread.[101]
The Cape York Health Council commented that across Cape York there is 'probably
only about 18 or so methamphetamine users' but the number of crystal
methamphetamine users is unknown. The Health Council further remarked that 'people
know it is around and report it, but [health services] are not seeing the worst
effects of [crystal methamphetamine] coming into the health services as yet'.[102]
The Cape York Partnership said that 'regions like Cape York are very vulnerable
to drugs like ice' and therefore its representatives were:
...very concerned about this drug and its potential consequences.
But it is 'potential'. We are not saying that ice is prevalent in use or
consequences at this stage in Cape York, thankfully.[103]
2.58
Overall, the committee was made aware of a heightened level of concern
amongst Indigenous communities about the risk posed by crystal methamphetamine
and the proactive approach taken by some communities. Dr Pendo Mwaiteleke from
the Cape York Partnership said that there had been a summit of:
...200 community leaders and representatives. One of the themes
that came across really strongly was that there is actually a growing culture
within the community and community leaders that they do not want ice in the
community and are trying to do everything to make sure that ice does not come
in. At the same time, there are some anecdotes that there have been some
attempts to bring ice into some communities. I made a visit to Aurukun. The
community is very strong. I spoke to quite a number of people, and everyone I
spoke to was very anti-ice. There was a feeling that, if ice were to get into
the community, it is going to be devastating. 'We are trying to solve the
problems that we have; so, if we do not stand up to make sure that ice is not
brought to our community, we know there are going to be very serious
ramifications'.[104]
2.59
The WA Primary Health Alliance informed the committee that there are two
principal concerns regarding crystal methamphetamine use in Indigenous
communities. Firstly, younger Indigenous people are more likely to develop
dependency issues; and secondly, high rates of crystal methamphetamine being
administered intravenously.[105]
As noted above, longitudinal studies confirm that these issues are mirrored in
the Australian population more broadly. However, the evidence indicates that
these issues, combined with the challenges faced by Indigenous communities,
increases the impacts of crystal methamphetamine use on young Indigenous
people.
2.60
The Aboriginal Health Council of Western Australia, when asked whether
crystal methamphetamine use more prevalent in Indigenous communities,
responded:
Throughout a number of consultations that we have undertaken
with our sectors, we have seen the shift and we have seen the impacts that
methamphetamines have. It has had an empowering or overwhelming effect on,
particularly, our younger generations. However, it is a combination of alcohol
and methamphetamine usage. Whilst there has been evidence provided that alcohol
use is still higher than methamphetamine use, in our opinion, looking at it
from the Aboriginal community perspective, we see methamphetamine use
overpowering alcohol use. One of the things that we have been adamant about is
that just focusing on methamphetamine use is not going to have a dramatic
impact, because we need to also deal with the social impacts for these young
people who actually have that urge to sample that particular drug.[106]
Lesbian, gay, bisexual, transgender
and intersex community
2.61
Another community that presents with higher use of crystal methamphetamine
is the lesbian, gay, bisexual, transgender and intersex (LGBTI) community. The AIHW
reports that people who identify as homosexual or bisexual are 4.5 times more
likely to use methamphetamine than people in the general population.[107]
2.62
The 2016 Sydney Gay Community Periodic Survey reports that since 2012
there has been a significant decline in the use of crystal methamphetamine,
although HIV positive men are disproportionately more likely to report using
the substance.[108]
Of the 3015 men surveyed, 10.4 per cent reported use of crystal
methamphetamine, down from the 11.5 per cent (2846 respondents) in 2015.[109]
2.63
The 2016 Gay Community Periodic Survey for Melbourne reported that
crystal methamphetamine use amongst Melbourne's gay population had remained
stable.[110]
In 2016, 9.9 per cent of the 2886 respondents reported using crystal
methamphetamine, lower than the 11.4 per cent (3 006 respondents) in 2015.[111]
2.64
The AIDS Council of New South Wales advised the committee that LGBTI
people may use drugs:
...for similar reasons as the general populations, the ways in
which this use plays out can be very different for people in [LGBTI]
communities. There is a significant association between the use of
methamphetamine and sex, and that use can impact negatively on sexual health
and HIV, both in terms of transmission and treatment adherence. This
association is very complicated and is worthy of dedicated and specific
government attention.[112]
2.65
The Penington Institute reported that HIV positive men who have sex with
men (MSM) and use crystal methamphetamine are 'more likely to report high-risk
sexual behaviours such as unprotected anal intercourse, compared to HIV
positive MSM who do not use ice'.[113]
The use of drugs such as crystal methamphetamine during sex has become commonly
known as 'chemsex' and is a growing sub-culture within the Australian LGBTI
community.[114]
2.66
Although use of crystal methamphetamine in the LGBTI community is
significantly higher than the general population, its use is not as visible, and
as a result of this lack of visibility:
...its use and impacts are often more private and hidden.
Despite this lack of visibility, the impacts can be just as great. They can
include loss of careers, relationship stress and domestic and family violence,
but rarely do they manifest in the displays of public aggression or dysfunction
that play out in other sections of the community.[115]
The mental and physical effects of crystal methamphetamine
2.67
Amphetamine and methamphetamine have similar effects; however differences
in the chemical structure of methamphetamine increase its potency.[116]
The short term mental effects of use may include:
-
anxiety;
-
fatigue;
-
irritability;
-
hallucinations;
-
suppressed appetite; and
-
insomnia.[117]
2.68
Long term mental effects may include:
-
memory loss;
-
decision making impairment;
-
drug dependency;[118]
and
-
depression, anxiety and psychosis.[119]
2.69
In the short term, the physiologically the effects of crystal
methamphetamine on the body include:
-
an increase in the user's heart rate;
-
hypertension; and
-
constriction of blood vessels.[120]
2.70
In the long term, the physical effects include:
-
an increased risk of stroke;
-
potential for ruptured blood vessels in the brain;
-
decreased lung function;
-
poor dental health;[121]
-
weight loss;
-
skin problems; and
-
sleep problems.[122]
2.71
In addition to the negative effects listed above, submitters noted that of
particular public concern are psychotic episodes and violent behaviour induced
by the use of crystal methamphetamine. These are discussed in greater detail in
the following sections.
Methamphetamine-induced psychosis
2.72
As highlighted by the Australian Drug Foundation (ADF), one of the more
serious health impacts of chronic methamphetamine[123]
use is psychosis. The symptoms of psychosis include confusion, delirium and
panic, which can be accompanied by a range of hallucinations.[124]
The ADF told the committee that users of methamphetamine are:
-
11–12 times more likely to experience psychosis than the general
population;
-
23 per cent more likely to experience clinically
significant psychotic symptoms of suspiciousness, hallucinations or delusions;
and
-
where they are dependent on methamphetamine, three times more
likely than their non-dependent peers to have experienced psychotic symptoms.[125]
2.73
A common manifestation of methamphetamine-induced psychosis is the delusion
of insect and/or parasite infestations under the user's skin.[126]
2.74
Professor McKetin explained that one risk associated with
methamphetamine use is an acute psychosis that manifests as transient paranoia
and 'when people are using this drug, their risk of that paranoid state
increases five-fold from when they are not using the drug'.[127]
A further risk is that transient psychosis for a minority of people can trigger
a more chronic psychological problem. However, there is less evidence to
support this idea and researchers 'do not know whether it has triggered
schizophrenia because they are already predisposed to schizophrenia, or whether
it is just a prolonged episode of methamphetamine psychosis that will
eventually go away'.[128]
Professor McKetin estimated that 20 per cent of users who have transient
psychosis will form some kind of chronic symptoms.[129]
2.75
A paper published by the National Drug and Alcohol Research Centre
(NDARC) in 2005 examined the Sydney methamphetamine market and reported that
psychotic episodes tend to last up to three hours and only 11 per cent of those
people who suffer psychosis attend hospital. Those people who attend hospital
were 'more likely to have more severe long lasting symptoms'.[130]
Of those users that displayed symptoms of psychosis, half felt 'hostile or
aggressive at the time, and one quarter of methamphetamine users exhibited
overt hostile behaviour while they were psychotic, such as yelling at people,
throwing furniture or hitting people'.[131]
2.76
In addition to psychosis, methamphetamine can have a long-term effect on
the cognitive function of users. Professor Roche said that it has a more
damaging effect 'than many other drugs' and:
...within a very short period of time it can severely impact on
your ability to think clearly and function, and it can take one to two years to
regain that normal cognitive functioning that you had previously. That is one
of the very severe potential outcomes of methamphetamine use.[132]
Violent behaviour
2.77
A significant concern for those in regular contact with crystal
methamphetamine users is severe aggression. Many representatives from law
enforcement agencies and frontline health and welfare services reported incidences
of violent behaviour to the committee.
2.78
The Victoria Police observed that some users of crystal methamphetamine
can become quite violent and that police have seen violent behaviour 'play out
in the street' between dealers and users. In comparison, those addicted to
heroin 'did not resort to the level of violence that [users] do with [crystal
methamphetamine]'.[133]
Victoria Police qualified 'that [the] demeanour of the individual probably
enhances it, but violence is a factor that [police] see in a lot of
individuals'.[134]
2.79
The Penington Institute informed the committee that people in the family
violence sector have reported extreme levels of violence associated with
crystal methamphetamine use. The problem, therefore:
...is that the connection between violence and ice is much more
complex than only those people who are addicted or only those people with a
severe problem. It could be people in their first period of use or it could be
someone with an extreme problem'.[135]
2.80
The issue of domestic violence was highlighted by the NDARC, which
argued that the discussion about crystal methamphetamine-related violence has to
date primarily focused on random acts of violence in areas such as Kings Cross.
However, little consideration has been given to domestic violence especially in
concert with alcohol. The NDARC said that it was rare to have an individual
that has taken only one drug and:
If you get a combination of alcohol with crystal
methamphetamine in a certain person who has a propensity for rage than you are
going to find yourself in a very difficult situation. So I think it is probably
not as simple as talking about one drug versus another drug. I think you get
this combination in people, and I think that combination or the effect of that
combination behind closed doors is unseen. We see the street assaults; we do
not see the family violence. I think that, for that very reason, we need to
focus more attention.[136]
2.81
Other submitters and witnesses cautioned against over-emphasising
violence associated with crystal methamphetamine use. In particular, a number
of submitters and witnesses highlighted that while crystal methamphetamine is a
dangerous drug that has significant health and social impacts on individuals
and communities, alcohol is a far bigger problem. For example, Professor Roche
stated that there are difficulties quantifying a greater propensity to violence
among users of crystal methamphetamine and that a number:
...of substances can induce more aggressive and violent
behaviours. Certainly you see it with the stimulants—say, with
methamphetamine—but we also see it with some individuals with alcohol as well.
We have exceptionally high levels of alcohol related violence in our community.
We do not have good data that can compare one group using alcohol and being
violent compared to people being intoxicated with methamphetamine. In both
instances they both become cognitively impaired and so their judgement is
really affected. With methamphetamine you have an elevated threat response. So
often it is not an issue of somebody wanting to behave in a violent and
aggressive way. The drug affects the brain in such a way that they cannot form
appropriate and accurate judgements about what is happening around them and
they feel very threatened and then often can lash out. People do behave quite
differently and it can manifest in violent behaviour in a way that is different
from other substances.[137]
2.82
Similarly, the APS opined that crystal methamphetamine is a problem,
however:
...alcohol
is probably an even greater problem. We are talking about a very low incidence.
I loved reading that submission from Emergency Medicine pointing out that the
number of more serious acute aggressive episodes in emergency departments are
not due to ice, they are due to people with alcohol. It is just that the people
with alcohol eventually fall asleep on you and the person with ice does not. At
the moment, we are certainly seeing sensationalism in this, but alcohol is
significantly more problematic than ice for emergency departments, police and
families.[138]
2.83
Indeed, Dr Wodak advised that:
The violence we see from alcohol at St Vincent's Hospital and
at every emergency department in every hospital throughout the country is
colossal. Every Thursday night, every Friday night and every Saturday night if
you go to any emergency department in the country between 9 pm and 3 am it is
mayhem—and it is largely caused by alcohol.[139]
Ambulance callouts and emergency
department presentations
2.84
Accurate information about ambulance callouts and emergency department
presentations associated with methamphetamine use is difficult to ascertain as
this data is not consistently collected by ambulance services and emergency
departments across the country. There are, however, a number of initiatives to
record this information that provide a valuable insight into the growth of methamphetamine-related
ambulance callouts and emergency department presentations. Two examples are
Turning Point's Ambo Project, which collects Victoria's ambulance callout data,
and the data collected by New South Wales (NSW) emergency departments.
Turning Point's Ambo Project
2.85
Turning Point's ongoing initiative titled Ambo Project: Alcohol and
Drug‑Related Ambulance Attendances records ambulance callout trends
and the substances involved. It began in 1998 in collaboration with Ambulance
Victoria and is funded by the Victorian Department of Health.[140]
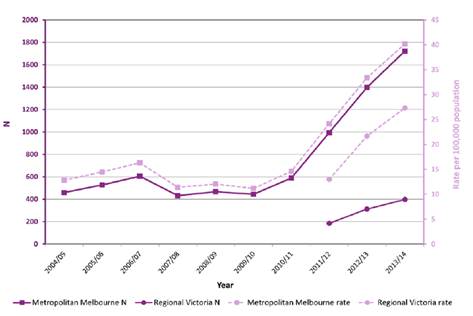
Data collected identifies crystal methamphetamine-related attendances. Evidence
presented in the Ambo Project's 2014–15 report shows a significant growth in
the total number of crystal methamphetamine attendances in Victoria between
2013–14 and 2014–15 with an increase of 47.8 per cent (see Table 10 and Figure
3).
Table 10: Number of attendances,
crystal methamphetamine, in metropolitan Melbourne and regional Victoria,
2013–14 and 2014–15[141]
|
Metropolitan Melbourne |
Regional Victoria |
All Victoria |
| 2013–14 |
1240 |
296 |
1537 |
| 2014–15 |
1802 (+45.3 per cent increase) |
467 (+57.8 per cent increase) |
2271 (+47.8 per cent increase) |
Figure 3: Crystal
methamphetamine-related attendances by year – 2004–05 to 2013–14[142]
![Figure 3: Crystal methamphetamine-related attendances by year – 2004–05 to 2013–14[142]](~/media/Committees/le_ctte/Crystalmethamphetamine45/First_report/c02_3.jpg)
2.86
Since data collection commenced in 2004-05, Victoria's all amphetamine‑related
ambulance attendances have increased with a notable upward trend since 2010–11 (see
Figure 4).
Figure 4: All amphetamine-related
attendances by year – 2004–05 to 2013–14[143]
2.87
The committee is aware that the National Ice Action Strategy (NIAS) supports
a commitment to expand the Ambo Project to all states and territories[144]
based on the National Ice Taskforce's (NIT) recommendation to establish 'a
system to gather and share national ambulance data drawing on the Victorian
'Ambo Project'.[145]
New South Wales emergency
department presentations
2.88
NSW emergency departments routinely collect data about methamphetamine
presentations.[146]
This data shows that there has been an increase in these presentations: in
2009–10 there were 470 people attending a NSW emergency department with a
methamphetamine-related presentation, in 2015–16 there were 4771 people (see
Table 11).
Table 11: Methamphetamine-related
NSW Emergency Department presentations, persons aged 16 years and over, 2009–10
to 2015–16[147]
| Year |
Number of persons |
| 2009–10 |
470 |
| 2010–11 |
699 |
| 2011–12 |
1162 |
| 2012–13 |
1834 |
| 2013–14 |
2455 |
| 2014–15 |
3627 |
| 2015–16 |
4771 |
2.89
Again, 2010–11 and 2011–12 mark significant upwards shifts in the number
of methamphetamine-related presentations to emergency departments.
Deaths linked to methamphetamine
use
2.90
During the course of the inquiry, the committee was told that deaths
linked to methamphetamine are considered quite rare.[148]
However, data from the 2016 household survey demonstrates that the public
increasingly believes that meth/amphetamine deaths are quite common. Survey
participants ranked meth/amphetamine as the third highest drug thought to cause
deaths in Australia (from 8.7 per cent in 2013 to 19.2 per cent in
2016), after tobacco (23.9 per cent in 2016) and alcohol (34.7 per cent in
2016).[149]
2.91
Available data has shown an increase in meth/amphetamine deaths. The
NDARC reported that accidental drug deaths involving methamphetamine significantly
jumped between 2010 and 2011. An examination of drug-related deaths, hospital
admissions and treatment services by The Guardian suggested that there
were 101 methamphetamine-related deaths in Australia in 2011, 16 more than in 2010.[150]
Estimates have also indicated that up to 170 drug-induced deaths involved
methamphetamine in 2013.[151]
2.92
On 28 March 2017, the Victorian Coroner released statistics on the
number of people who had died in Victoria from drug overdoses. Since 2009,
Victoria has seen the number of drug overdose deaths steadily increase. In
2016, instances where methamphetamine contributed to an overdose death
increased by 40 per cent, from 72 to 116 people. Seventy per cent of
all fatal overdoses in Victoria have been contributed to poly-drug use.[152]
2.93
A further study was released by the NDRI on 31 July 2017. The NDRI
assessed 1649 crystal methamphetamine related deaths between 2009 and 2015 and
found 43 per cent of those deaths were caused by an overdose; 22 per cent of
deaths were due to natural diseases, such as heart disease. The study found the
yearly national death toll had doubled between 2009 to 2015, most of which
occurred in rural and regional areas (41 per cent).[153]
2.94
The NDRI's Professor Shane Darke said the results show that crystal
methamphetamine 'is a serious public health problem and I think we're right to
treat it as such. This is not a beat-up, this is real'.[154]
Professor Darke noted that the number of deaths due to crystal methamphetamine
appeared to have stabilised, but have stabilised at a worrying level.[155]
2.95
Although the rise in deaths related to methamphetamine is a concern,
Professor Roche made a comparison between methamphetamine and the heroin
epidemic in the 1990s:
It is probably helpful to remind people that, in 1999 in
Australia, 1,000 young Australians died from a heroin overdose. That is pretty
catastrophic. I think it is helpful to keep a balance here. We have in
Australia dealt with numbers of very severe drug problems. Death is as catastrophic
as it is going to get, and we know that the death rate associated with
methamphetamine is increasing. So death is the worst possible outcome, and that
is the thing that we work extremely hard to prevent. We then work back in terms
of a hierarchy of harms after that.[156]
Drivers of crystal methamphetamine use
2.96
Despite the negative emotional and health effects of meth/amphetamine
use, people continue to use these drugs throughout Australia. Reasons for
consuming meth/amphetamine, include to:
-
increase productivity (especially in work environments);[157]
-
increase pleasure and enjoyment (including sexual activities);
-
manage emotions;
-
increase a sense of belonging;
-
replicate perceived 'normative' behaviour;
-
expand one's consciousness/heightened awareness; and
-
counter the effects of other drugs and/or avoid the negative
experience of drug withdrawal.[158]
2.97
As described in the ADF's 2015 report Drugs: the facts:
People use drugs to relax, to function, for enjoyment, to be
part of a group, out of curiosity or to avoid physical and/or psychological
pain. Drug use is influenced by a number of factors. Most people use drugs
because they want to feel better or different. They use drugs for the benefits
(perceived and/or experienced), not for the potential harm. This applies to
both legal and illegal drugs.[159]
2.98
Another significant driver of methamphetamine use in Australia is
inequality. The Ted Noffs Foundation called crystal methamphetamine 'a drug
of disadvantage'.[160]
Typically, as with other drugs such as heroin, disadvantaged communities
experience the negative impacts of crystal methamphetamine more so than
advantaged communities. According to the Ted Noffs Foundation,
approximately 80 per cent of their clients are socially and economically
disadvantaged.[161]
Important factors identified by the Ted Noffs Foundation as contributing to
this trend include:
-
intergenerational drug use and children baring witness to the
dysfunctional use of drugs and alcohol;
-
community drug usage that normalises that behaviour for children;
-
people who experience homelessness;[162]
and
-
the difficulties for children to remove themselves from these at
risk communities.[163]
2.99
The ADF also identified that those people most at risk of problematic
drug use are vulnerable through 'no "fault" of their own' and are
significantly influenced by both environmental and biological factors outside
of their control.[164]
These factors include:
-
the emotional distress caused by the lack of employment
opportunities, or mental health problems;
-
children with learning difficulties and dysfunctional family
environments; and
-
the lack of positive role models to guide young people to make
constructive life choices.[165]
2.100
Professor McKetin said there would always be a proportion of the
Australian population that will 'indulge in drug taking, and that is related to
social acceptability of drug use, availability of drugs, and a variety of other
factors'.[166]
However, Professor McKetin emphasised that one key predictive factor in
determining whether an individual develops a dependency for an illicit drug is
that person's resilience.[167]
2.101
Professor McKetin listed other factors that may contribute to a user
developing a problematic drug habit:
Things like mental health problems, low socioeconomic status,
lack of opportunities, all of these things increase the risk of drug problems
developing, as does the availability of the drug in the community, and this is
not to be underestimated because now we have high availability of this drug.[168]
2.102
Dr Wodak highlighted the importance of discussing the role of inequality
in the context of these public health problems, and argued:
A number of public health researchers around the world have
come to the conclusion that countries with high levels of inequality—and that
includes Australia—have much higher levels of mental health and public health
problems such as illicit drug use. It is striking when you compare Australia, a
country with high inequality, to Japan and the Scandinavian countries, which
have much lower levels of inequality. In all those countries the problems they have
with illicit drugs are a fraction of the problems we experience in Australia.
Proving this hypothesis is probably beyond us, but the face validity is such
that we should be doing it.[169]
2.103
The Penington Institute suggested that another contributing factor to
Australia's high levels of methamphetamine consumption is the demand for
intoxication through drugs (both legal and illegal) and opined that 'we have to
deal with the driver for drug consumption, which is, indeed, ourselves. It is
the Australian community; it is not a failure of law enforcement. It is a
failure of the community'.[170]
Price, purity and methods of administration
2.104
The following sections of the report discuss the price, purity and
methods of administration of crystal methamphetamine, and how these have
changed over time.
Price
2.105
The ACIC's Illicit Drug Data Report 2015–16 revealed that the
price of crystal methamphetamine continues to decline, despite record seizures.
Crystal methamphetamine's price per gram across the nation ranged from
$150 to $1200, down from $250 and $1200 per gram in 2014–15.[171]
The price per gram in 2013–14 was $300 to $1600.[172]
It was also reported that a point (a tenth of a gram)[173]
of crystal methamphetamine cost around $20 to $200, compared to $50 to $150 in
2014–15.[174]
2.106
Nationally, in 2015–16 the price per kilogram for crystal
methamphetamine ranged from $75 000 to $280 000 in 2015–16. The price range in
2014–15 was between $120 000 and $280 000.[175]
2.107
Professor McKetin discussed the relationship between the price per
'point' and the availability of crystal methamphetamine. She advised that
crystal methamphetamine's price (in the Sydney market) has remained relatively
stable, suggesting that price has not been a factor driving increased usage:
...the price seems to have been $50 a point forever, at least
in Sydney, and what changes is the purity, the availability. I am sure that
there is a relationship. We saw it with heroin, and it was about the dose
relationship and the way it was marketed as well. It went from something that
you could buy as a gram from a secret dealer that you would have to know
personally for a few hundred dollars, and then the price dropped down to about
$200, which was cheap for a gram, but what happened was that people started
selling it on the street corner for $20 or $30 a cap. That makes it much more
accessible...I actually could imagine common sense is like, if you can pay a certain
amount of money for a drug that is going to give you a good high for four
hours, and you look at the price of alcohol and other drugs, it is going to
play a role.[176]
Purity
2.108
Although the price of crystal methamphetamine continues to decline, the
purity of crystal methamphetamine has increased.
2.109
The Illicit Drug Data Report 2015–16 outlines the median purity
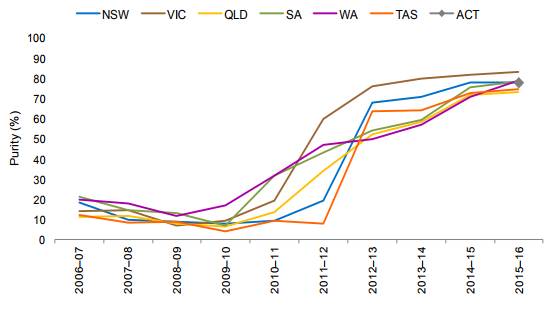
of amphetamine/methamphetamine samples from 2006–07 to 2015–16. Figures 5 and 6
are drawn directly from the report and demonstrate that the purity of methamphetamine
samples in particular have increased drastically between 2010–11 and 2015–16.
Figure 5: Annual median purity of
amphetamine samples, 2006–07 to 2015–16 (by state and territory)[177]
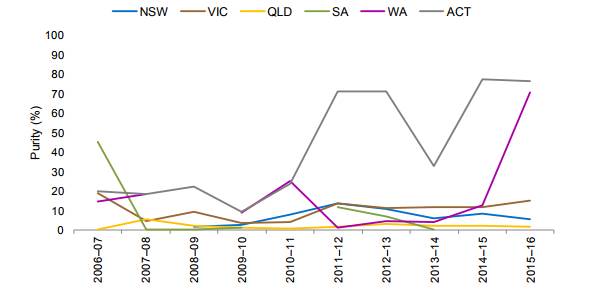
Figure 6: Annual median purity of
methamphetamine samples, 2006–07 to 2015–16 (by state)[178]
2.110
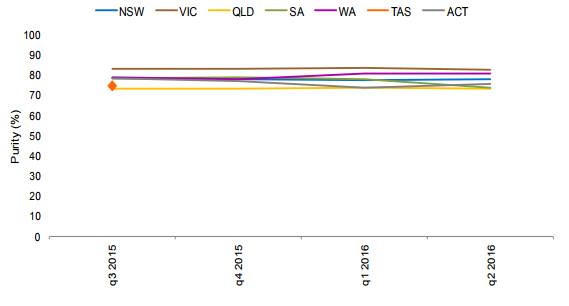
The quarterly analysis of the median purity of methamphetamine samples
in 2015–16 (by state) (see Figure 7) indicates that most states have
methamphetamine with purity between 70 to 80 per cent, and that this level
of purity remained stable over the course of the year.
2.111
Participants in the 2015 IDRS remarked that the purity of crystal
methamphetamine was 'high' and that high purity methamphetamine was considered
'easy' and 'very easy' to obtain.[179]
2.112
A number of submitters discussed the purity of crystal methamphetamine,
with many highlighting the increase in purity as a significant concern.
2.113
The NDARC highlighted that crystal methamphetamine is becoming the preferred
form of methamphetamine and is increasing in purity, observing:
...the community has moved towards a changed form of the
substance. Where traditionally we had seen the powder form more commonly used,
we have seen a move towards ice in its crystalline form. That doubled in that
population survey in 2013 that we were talking about. That means we are seeing
more people taking the crystalline form, which is a purer form, but they are
also taking that form more regularly. They are using it more often. We know
from a lot of previous work that the crystalline form is generally of much
higher purity than the powder form or any of the other forms. If you have an
increase in the pure substance being taken more often then you are going to
find the potential for harm is, indeed, magnified.[180]
Figure 7: Quarterly median purity
of methamphetamine samples, 2015–16 (by state)[181]
2.114
Additionally, the Centre for Population Health at the Burnet Institute spoke
of users not necessarily knowing the purity of crystal methamphetamine each
time it was purchased, a situation that can cause greater harm to the user and
the community. Work done by the Burnett Institute shows:
...when someone goes and buys the drug, and they are buying a
typical amount, they are typically buying, say, 0.1 of a gram. When they used
to purchase it a few years ago, it used to be around 15 per cent pure, and it
would cost a certain amount. Then through the end of 2013, the price they paid
went up a little bit, but the purity had gone up from, say, 15 per cent to
around 70 per cent. So essentially for the same amount of money, you would get
a dramatically increased amount of the drug. People who were not used to using
such high purity drugs were getting into much more trouble, and that is a
really plausible explanation for the increase in ambulance call-outs, the increase
in emergency department presentations, and all of those harms that you
mentioned in the health domain would easily be accounted for by that change in
purity, as well as the change from using powder through to using the crystal
form of the drug, which generally is smoked.[182]
Methods of administration
2.115
Crystal methamphetamine is typically administered into the body either by
smoking (through a glass pipe) or injecting directly into the bloodstream.
According to the School of Social and Political Science at the University of
Melbourne, these two forms of use are 'extremely efficient absorption
mechanisms...which means you get a bolus dose—a big thump of the drug straight
away...[t]hat is going to be a much more intense experience than someone who
snorts the drug'.[183]
As noted by Burnet Institute:
If you smoke the drug, the way in which it is metabolised, or
the body takes it up, the effect is much quicker than if you were to snort it,
as people traditionally did with speed powder.[184]
2.116
Professor McKetin agreed that because crystal methamphetamine is
primarily smoked, it has become a social drug, unlike injecting methamphetamine,
which is a stigmatised behaviour. The ease of passing around a pipe to smoke
crystal methamphetamine means users:
...take it to a party and bang, 20 people are exposed to it. It
is also because when someone becomes dependent, the main way that they will
earn the money to support their drug habit is through dealing. That way they
get a ready supply of wholesale price methamphetamine. In doing that, they sell
it to their friends...That is how the market operates. If you have someone who is
dependent, it is a social drug; they take it to the party and then they start
selling it to those friends. There is a potential for this to spread more
rapidly than what we would have seen with other forms of the drug, because you
have the dependence liability and you have the social aspect.[185]
Poly-drug use
2.117
Poly-drug use—which involves the use of multiple substances at once—is another
issue commonly associated with crystal methamphetamine, especially problematic
users, who 'dabble across a range of substances and are polydrug users'.[186]
2.118
The committee heard that poly-drug use, including crystal
methamphetamine, was a common feature of people seeking treatment for drug
addiction. The Salvation Army placed emphasis on this fact, stating that it
does not generally see methamphetamine use in isolation:
Once people get into treatment services they are usually
polydrug users, so it is very rare to get someone who has only used ice. Very
often we will see people having used opiates such as heroin or benzodiazepines
such as valium to assist them in the cycle of ups and downs; they would use one
of those other drugs to help them come off. Of course, alcohol and ice are quite
a difficult combination we see a lot of, particularly because people are able
to drink a lot more alcohol without feeling drunk while they use ice. The
increased complexity in related health issues is a huge issue for us as well.[187]
National data on illicit drug arrests and illicit drug offences recorded in
Australia's criminal courts
2.119
The ACIC's Illicit Drug Data Report for 2015–16 shows that the
number of illicit drug arrests in Australia have continued to rise over the
last decade. There were 82 389 arrests in 2006–07; the total increased to 154
538 arrests in 2015–16 (an 87.6 per cent increase).[188]
By drug, the ACIC reported the following:
-
National ATS arrests have increased by 213 per cent over the last
decade, with 15 216 people arrested in 2006–07 and 47 625 people arrested
in 2015–16. Proportionally, ATS arrests make up 30.8 per cent of all
national illicit drug arrests, a substantive increase from 18.5 per cent in
2006–07.
-
The number of cannabis arrests have increased by 40.1 per cent
over the last decade, with 56 862 people arrested in 2006–07 and a record 79
643 people arrested in 2015–16. Proportionally, this total has decreased from
69 per cent of all drug arrests in 2006–07 to 51.6 per cent in 2015–16.
-
Heroin and other opioid arrests have increased by 37.5 per cent,
from 2164 in 2006–07 to 2975 in 2015–16. However, as a proportion of all drug
arrests this total has decreased from 2.6 per cent in 2006–07 to 1.9 per cent
in 2015–16.
-
The number of cocaine arrests has increased by 270.8 per cent,
from 699 in 2006–07 to 2592 in 2015–16. Proportionally, these arrests represent
0.8 per cent of all drug arrests in 2006–07 and 1.7 per cent in
2015–16.
-
Other and unknown drug arrests have substantially increased too,
by 191.4 per cent over the past decade. In 2006–07 there were 7448 arrests and
in 2015–16 there were 21 703 arrests. As a proportion of all drug arrests this
has increased from 9 per cent in 2006–07 to 14 per cent in 2015–16.[189]
2.120
Figure 8 shows the number of national illicit drug arrests from 2006–07
to 2015–16 by drug type.
Figure 8: National illicit drug
arrests by drug type, 2006–07 to 2015–16[190]
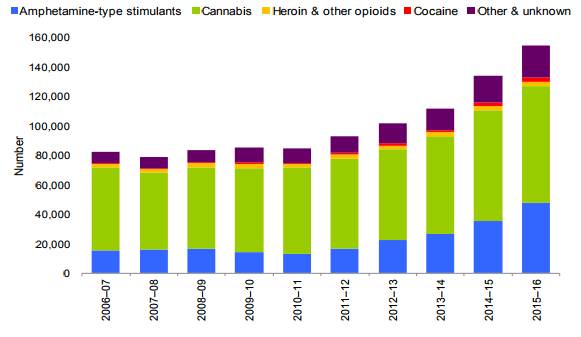
2.121
The growth in the number of arrests has correlated with an increase in
the number of illicit drug offences (including charges for possession and use)
recorded in the criminal courts of each state and territory. The Australian
Bureau of Statistics (ABS) provides this data annually. Although this data does
not distinguish between drug types, it does provide insight into the broader
context of illicit drug use and possession offences in each state and
territory.
2.122
Key findings from Australian criminal courts for 2015–16 revealed the
number of defendants finalised[191]
for an illicit drug offence has continued to rise. In 2015–16 there were 63 541
defendants finalised with a principal offence for an illicit drug offence(s),
an increase from the 59 341 finalised offences in 2014–15. The majority, 59 per
cent (37 201) of these 'defendants were charged with offences related to
possession or use of illicit drugs'.[192]
2.123
The increase in the number of defendants finalised for possession and
use of illicit drugs was highlighted by the ABS on 1 March 2016. The ABS
reported the number of defendants finalised for illicit drug offences in
2014–15 had continued to rise, and were at the highest level in the past five
years. The 2014–15 figures show an increase of 51 per cent compared to 2010–11.
Fifty eight per cent of those finalised for illicit drug offences in 2014–15
were for possession and/or use.[193]
The ABS reported possession/use offences have increased by 21 per cent (5834
defendants in total) compared to 2013–14.[194]
Seventeen per cent of illicit drug offences that were finalised were for
dealing or trafficking illicit drugs. These increases continue an upward trend
in the number of illicit drug cases before Australian courts. [195]
2.124
Nationally in 2015–16, there were 56 282 defendants proven guilty for
illicit drug offences. Of this total, 35 578 were for possession and/or use
offences.[196]
2.125
Table 12 shows national illicit drug offences for defendants proven
guilty by offence type, from 2008–09 to 2015–16.
Table 12: National illicit drug offences
for defendants proven guilty by offence type, 2008–09 to 2015–16[197]
| Year |
2008–09 |
2009–10 |
2010–11 |
2011–12 |
2012–13 |
2013–14 |
2014–15 |
2015–16 |
| Illicit drug offences (total) |
34 555 |
35 713 |
33 894 |
35 447 |
38 914 |
44 788 |
52 561 |
56 282 |
| Import or export illicit drugs |
139 |
191 |
161 |
217 |
191 |
253 |
228 |
186 |
| Deal or traffic in illicit drugs |
4792 |
4736 |
4463 |
4684 |
4753 |
5678 |
6262 |
7106 |
| Manufacture /cultivation of illicit drugs |
4806 |
5066 |
5037 |
4877 |
4578 |
5085 |
4964 |
4519 |
| Possession and/or use of illicit drugs |
21 136 |
21 667 |
20 380 |
21 494 |
24 214 |
27 145 |
32 712 |
35 578 |
| Other illicit drug offences |
3678 |
4053 |
3848 |
4178 |
5169 |
6620 |
8394 |
8888 |
2.126
The ABS also provides data on the number of defendants finalised for
principal illicit drug offences in each Australian jurisdiction. Table 13
shows annual figures of defendants finalised for a principal illicit drug
offence in the criminal courts of each state and territory, 2011–12 to 2015–16.
Table 13: Annual figures of
defendants finalised for a principal illicit drug offence in the criminal
courts of each state and territory, 2011–12 to 2015–16.[198]
| Year |
2011–12 |
2012–13 |
2013–14 |
2014–15 |
2015–16 |
| New South Wales |
| Illicit drug offences |
10 990 |
11 935 |
12 849 |
14 956 |
16 445 |
| Victoria |
| Illicit drug offences |
4147 |
4461 |
5010 |
5543 |
5499 |
| Queensland |
| Illicit drug offences |
14 429 |
16 229 |
20 120 |
23 970 |
25 158 |
| South Australia |
| Illicit drug offences |
3282 |
3573 |
3688 |
3310 |
3223 |
| Western
Australia |
| Illicit drug offences |
5787 |
6420 |
7740 |
9841 |
11 394 |
| Tasmania |
| Illicit drug offences |
1 127 |
895 |
720 |
797 |
820 |
| Northern
Territory |
| Illicit drug offences |
654 |
768 |
580 |
773 |
831 |
| Australian
Capital Territory |
| Illicit drug offences |
180 |
137 |
150 |
148 |
164 |
Committee comment
2.127
It has traditionally been difficult to get an accurate picture of the
extent of crystal methamphetamine use in Australia due to weaknesses with data
collection methods, largely surveys, and the likelihood of respondents
under-reporting drug use. For example, the AIHW household survey is susceptible
to under-reporting arising from negative popular views and media reporting that
may influence drug users' willingness to accurately self-report illicit drug
use. However, new approaches to data collection and analysis, such as the National Wastewater
Drug Monitoring Program, mark a significant step forward in gaining a more
thorough understanding of drug use in this country. The committee anticipates that
future wastewater analysis by the ACIC will build a more accurate picture of
drug use in Australia and assist governments, service providers and academics
to develop more targeted policies and strategies to address illicit drug use.
2.128
Crystal methamphetamine use is not necessarily a one way path to more
problematic consumption for all users. However, the drug can have serious
short- and long-term physical and psychological impacts and these should not be
under-estimated.
2.129
As demonstrated in this chapter, specialists have identified groups
within our community that are more at risk of developing problematic crystal
methamphetamine use and face greater hurdles when attempting to access
treatment. For this reason, culturally appropriate AOD resources must be
directed towards and treatment available to vulnerable communities, that is Australia's
young people, regional and remote communities, Indigenous communities and the
LGBTI community.
2.130
The committee also heard that problematic crystal methamphetamine use
has been linked to social and economic disadvantage and inequality. The
committee agrees that this is a feature of crystal methamphetamine use in
Australia and one that brings a complex dimension to the problem. However, it
can be glib to say that socioeconomic disadvantage and inequality cause
problematic drug use and the committee is concerned that this can have the
effect of further stigmatising or marginalising crystal methamphetamine users
on account of their socioeconomic circumstances. Genuine and serious
consideration must be given to the inter-relationship between people's
socioeconomic circumstances, their drug use and their ability to access AOD
services and treatment. In the committee's opinion, drug users' socioeconomic
status must be used to inform appropriate and effective policy responses and must
not simply be used to identify a particular group of drug users.
2.131
The committee is concerned that despite large, and in some cases record
seizures occurring at Australia's borders, the price, purity and availability
of crystal methamphetamine remains cheap, high, and readily accessible. In no
way does the committee wish to diminish from the efforts and successes of our
law enforcement and border protection agencies; however, the evidence before it
suggests to the committee that law enforcement strategies alone will not solve
the crystal methamphetamine problem in Australia.
2.132
Indeed, Mr Ken Lay APM, Chair of the NIT, announced at the release of
the NIT's final report that 'ice use is not a problem we can solve overnight,
and not something we can simply arrest our way out of'.[199]
The committee shares this view. The NIT and the NIAS appear to mark a
significant shift in and a renewed focus on Australia's national drug strategy,
and an attempt to rebalance the three pillars (supply, demand and harm
reduction). Submitters and witnesses to the inquiry, from both the health and
law enforcement sectors, consistently told the committee that crystal
methamphetamine use should be approached primarily as a health issue and not a
law enforcement issue.
2.133
The subsequent chapters of this report and the committee's second report
will consider current and future responses to crystal methamphetamine use in
Australia. In particular, the remainder of this report will focus on law
enforcement strategies and their effectiveness.
Navigation: Previous Page | Contents | Next Page