Issue
Australians spend over $7.6 billion a year on dental
services, which are not covered by Medicare. Nearly a fifth of Australians have
delayed or avoided necessary dental care due to cost. This scenario has led to
increased calls for the Australian Government to provide additional funding or add
dental services to Medicare. Historically, there have been contested views
about Commonwealth funding to improve dental service affordability and access,
and the way forward is still being debated.
Key points
- Most
dental services in Australia are funded by individuals, with some assistance
from private health insurance.
- State
and territory governments deliver targeted public dental services to children
and concession card holders.
- The
Australian Government contributes funding towards basic dental services for
eligible children. It also supports state and territory dental services
through public hospital funding and indirectly through the private health
insurance rebate.
- The
history of dental funding reform is largely a sustained debate over the
Commonwealth’s role and includes discussion about universal versus targeted
approaches.
- While
cost is a major barrier to reform, opportunities for targeted approaches
exist, such as for seniors and Aboriginal and Torres Strait Islander peoples.
Context
Who pays (and can’t pay) for dental services?
In 2022–23, $12.5 billion was spent
on dental services in Australia. Individuals spent more than $7.6 billion,
health insurers close to $2.5 billion, the Commonwealth nearly $1.4 billion,
and state and territory governments nearly $1 billion (Figure 1).
Concern about dental
affordability and access is long-standing. The Australian
Bureau of Statistics reports that in 2023–24, 17.6% of people delayed or
avoided seeing a dental professional due to cost (Table 14.3). This was
exacerbated for people in areas of most socio-economic disadvantage (27.3%) or
with a long-term health condition (20.8%) [see Table 15.2].
Figure 1 Percentage share of dental spend
2022–23
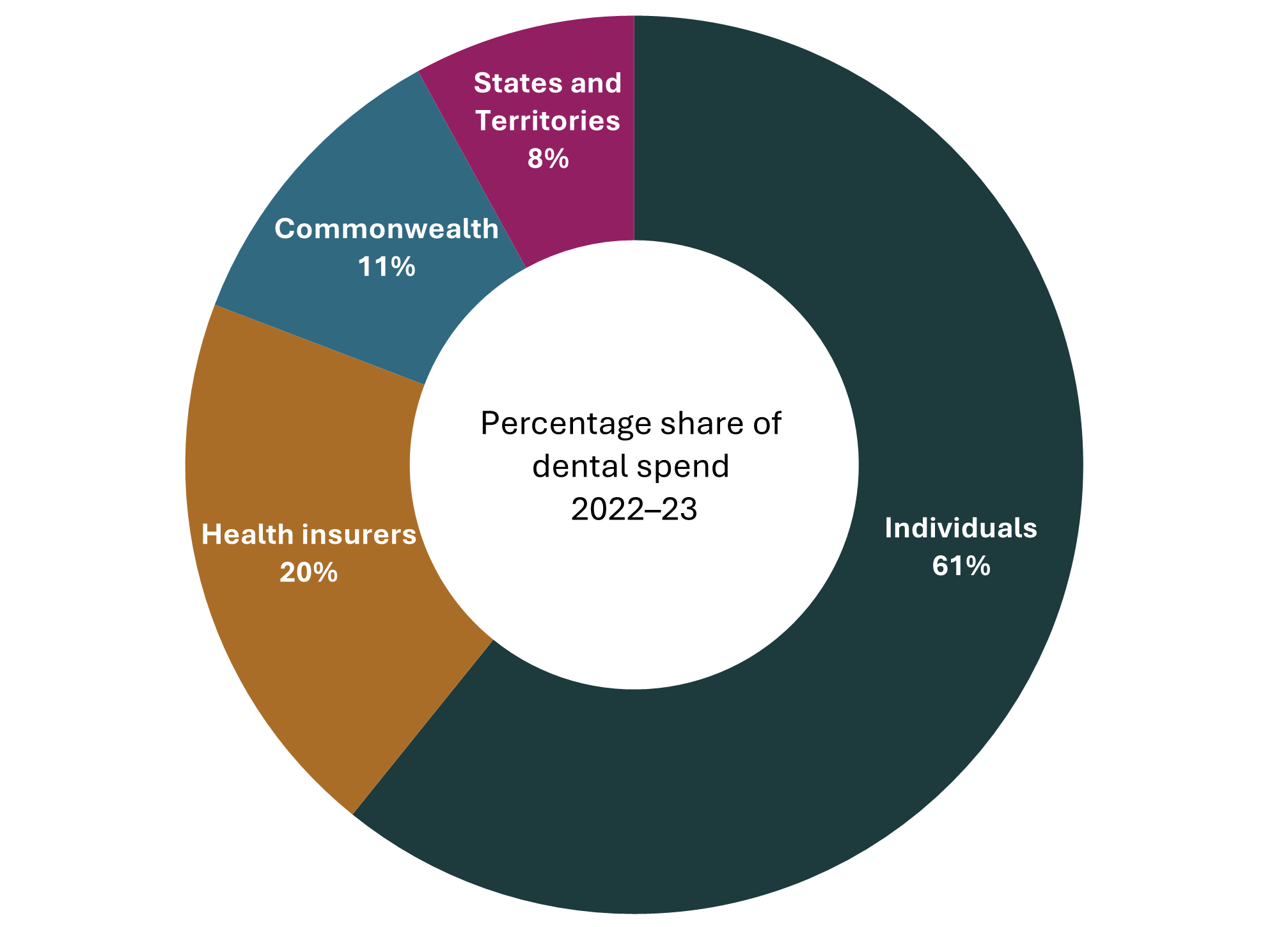
Source: Parliamentary Library graph using data from the Australian
Institute of Health and Welfare.
Current arrangements for Commonwealth funding of
dental services
Table 1 outlines key current Commonwealth dental funding
arrangements.
Table 1 Selected Commonwealth
funding for dental services
| Activity |
Description |
Mechanism |
Level of
funding |
Number of
people benefitting |
|
Child Dental Benefits Schedule (CDBS)
|
The
Commonwealth provides means-tested capped benefits (up to $1,132a over 2 years) for basic dental services (excludes orthodontic, cosmetic or in-hospital
dental services) delivered by private or public providers to children aged
0–17 years.
|
Dental Benefits Act 2008
Dental Benefit Rules 2014
|
Estimated
$325.9 million in 2025–26
(p. 76)
|
In 2021,
2,607,949 children were eligible; 959,517 used the CDBS (36.8%) (p. 13).
|
|
Funding to the states and
territories for adult public dental services
|
The Commonwealth provides
funding to the states and territories to support the delivery of additional
public dental services to eligible adult dental patients.
|
Federation Funding Agreement – Health – Public
Dental Services for Adults 2023–25b
|
$107.8 million in 2025–26c (p. 43)
|
Up to an additional
180,000 eligible dental patients are funded per year (based on 2023 figures).
|
|
Contribution to public hospital funding
|
The Commonwealth
contributes funding to states and territories for each episode of public
hospital dental services (admitted and outpatient).
|
National Health Reform Agreement
|
Estimated $178.8 million
in 2020–21; $125.4 million in 2021–22 (calculated from Table 1)
|
Not available.
|
|
Private health insurance (PHI) rebate
|
The Commonwealth provides
an income-tested rebate to help meet the costs of premiums for hospital, general
treatment (including dental) and ambulance policies.
|
Private Health Insurance Act 2007
|
Estimated $825 million in
PHI rebate paid out in dental claims in
2022–23 (Table A3)
|
Precise numbers of people
accessing dental rebates are not routinely published, but 55.1% of the population (more than 15 million people) have general
treatment (extras) cover. Singles earning above $158,000 and families earning above $316,000 are not eligible for any
rebate.
|
|
Rebates for veteran gold and white card
holders
|
The Commonwealth provides
rebates to providers via the Veterans dental schedules. Veteran Gold Card holders receive treatment based on clinical need, and Veteran
White Card holders receive treatment in relation to accepted
disabilities.
|
National Health Act 1953
|
Estimated $90 million in
2022–23 (Table A3)
|
Precise numbers of
veterans accessing dental rebates are not routinely published. As at September 2023 there were 104,543 Gold Card holders and 89,273 White Card holders.
|
a Benefit
cap if 2025 is the first year of the 2-year period. The cap amount is
indexed yearly on 1 January.
b The 2025–26
Budget provided $107.8 million in 2025–26 to extend the existing agreement
to 30 June 2026 (p. 52). An amended agreement has not been published.
c Under successive
agreements, annual funding has remained largely constant since 2017–18.
The Medicare Benefits Schedule funds some limited dental-related
services, such as treating patients
with an eligible
cleft and/or craniofacial condition. In 2024, this incorporated
approximately $9.6
million in benefits. The Commonwealth also
provides grants (pp. 2–3) to:
- Royal
Flying Doctor Service dental outreach services (around $5.8 million per year),
- population
health dental research studies (estimated $2.3 million between 2023–24 and
2025–26)
- some
targeted funding for Aboriginal and Torres Strait Islander people.
History of Commonwealth funding for dental services
Over the past 50 years, Australian governments have
introduced and abolished a range of dental initiatives. In 1946 a constitutional
change gave the Commonwealth powers to legislate with respect to providing
dental services. However, successive Australian governments have generally
regarded public dental services as state and territory responsibilities:
- The
1973–74 Federal Budget provided
funding for a national school dental scheme (p. 78) but it was subsequently
abolished in the 1981–82
Budget.
- Dental
services were excluded from Medicare and its predecessor, Medibank, which
commenced in 1975. Former Department of the Prime Minister and Cabinet
Secretary, John Menadue, reported
this was due to cost and anticipated resistance from the dental profession.
- In
1994 the Federal Government introduced the Commonwealth
Dental Health Program, providing funding to the states and territories
towards emergency and general public dental services. This was abolished from 1
January 1997 on the basis that the program had
met the original target of 1.5 million people (p. 75).
- The
2004–05
Federal Budget included an Allied Health and Dental Health Care Initiative as
part of the MedicarePlus package (p. 208). This provided for up to 3 annual dental
consultations for those with dental problems significantly exacerbating chronic
medical conditions. In response to low
take-up rates, the 2007–08 Budget expanded benefits (pp. 9–10).
- In
June 2008 the Government legislated a Medicare
Teen Dental Plan; however, the Senate
blocked its efforts to replace the previous Commonwealth dental scheme with
a new
promised program. The Coalition supported the existing scheme, while the
Greens called for additional government funding for those with chronic
illnesses (p. 2). An eventual
compromise led to a National Partnership Agreement, providing additional
funding to the states and territories, and an expanded CDBS replacing the Teen
Dental Plan. These negotiated reforms reflect the Commonwealth dental
commitments in place today.
- In
2016, the Federal Government proposed a new
Child and Adult Public Dental Scheme for concession card holders to replace
the CDBS and National Partnership Agreement. The Commonwealth would contribute
40% of funding (capped to CPI growth and population after an initial transition
period) but the states and territories would be responsible for program
delivery (pp. 102–103). Following criticism from dental
stakeholders
and the Opposition,
and a lack of support from some states, in December 2016 the Health Minister announced
the proposal would not proceed.
Reform debate
Brief history of reform proposals
Alongside these practical reform challenges have been the
more conceptual arguments regarding the Commonwealth’s role in funding dental
services. Some advocate for dental services to be a
universal entitlement incorporated into Medicare. Others have argued for more
targeted schemes providing free or low-cost dental services based on need.
Several inquiries have explored extending Medicare to
include dental treatment based on universal access principles. These include
the Layton
inquiry in 1986, 2 Senate inquiries (in
1998 and 2003)
– and a House of Representatives inquiry
in 2006. The most recent is the 2023 Senate Inquiry on the Provision
of and Access to Dental Services in Australia.
Proposals for targeted access to dental services involve
limited free or subsidised access based on means-testing or population features
such as age. The CDBS uses this targeted approach, which provides a potential
delivery model.
Examples of targeted access proposals include the
Australian Greens’ 2011
plan to phase in Medicare-funded services over 5 years, giving priority to
children and teens, the elderly, low income earners and those with chronic
diseases. The Greens reannounced versions of this policy in 2013,
2016
and 2019.
The 2012 report of the National
advisory council on dental health canvassed a range of targeted
arrangements, and several Senate inquiries have also recommended targeted
approaches, including in 1998
and 2023.
The Royal
Commission into Aged Care Quality and Safety (Recommendation 60) and the
2023 Senate
inquiry (Recommendation 13) recommended a Seniors Dental Benefit Schedule
modelled on the CDBS.
Universal access proposals to basic dental services, such as
check-ups and fillings, have included:
What now?
The costs of increasing public access to primary dental
services are regularly cited as a major barrier to reform in Australia. These
costs are significant, with the Parliamentary Budget Office estimating
that including dental
in Medicare could cost $45 billion over 3 years from 2025–26. Additionally,
a specific seniors
scheme across 10 years from 2024–25 could cost $15.6 billion capped or
$19 billion uncapped (pp. 17–20).
During the 2025 election campaign, Prime Minister Anthony
Albanese stated that the argument against fully including dental into Medicare
was ‘economic’
(pp. 9–10). Minister for Health and Ageing, Mark Butler, expanded
on this at a press club debate (pp. 12–13):
…although Labor has in its platform
and [sic] ambition to bring dental into Medicare more broadly, we don't have
the capacity to do that in the immediate future. … [W]hen we were last in
government, we introduced a Medicare style funding system for kids from
families receiving family tax benefit. That's working terrifically well...
There is a recommendation to consider an equivalent style scheme for seniors
that would be interesting to look at. Very expensive, but interesting to look
at.
Commonwealth, state and territory health officials have also
been discussing dental funding reform, including options
for public dental arrangements that better meet the needs of seniors and
Aboriginal and Torres Straight Islander peoples (p. 2).
Debate continues on the future
of dental funding reform, including on whether to pursue universal coverage or
continue refining targeted schemes, and how to best address growing concerns about
access to essential dental care for vulnerable groups.