4
August 2017
PDF version [397KB]
Amanda
Biggs
Social Policy Section
Introduction
The financing arrangements for health care in Australia are
complex, reflecting both historical developments unique to Australia and its federal
system of government.
Australia's health system is a mix of public and private
health care. Broadly, publicly-financed health care primarily refers to
services funded through government programs such as Medicare and the
Pharmaceutical Benefits Scheme, as well as public hospital services that are
jointly funded by the Commonwealth and the states and territories. In addition,
some health services are funded through private health insurance, individual
out-of-pocket payments, and third party insurers such as motor vehicle insurers.
It is not mandatory to have private health insurance cover.
Under Medicare,
all Australians are eligible for subsidised medical treatment and free treatment
as a public patient in a public hospital. However, private health insurance
provides a choice of doctor, can help with the cost of treatment in a private
hospital, and the cost of ancillary
treatments not covered by Medicare such as dental, optical and physiotherapy.
This quick guide outlines the broad arrangements around
private health insurance that exist today. It provides brief information on the
industry and regulatory arrangements, private health insurance membership and
types of cover, government surcharges and incentives, and key features of
private health insurance in Australia.
Current private health insurance
arrangements
Private health insurance sector
The origins of private health insurance lie in the friendly
and mutual societies that developed in the 19th century, which, for a
contributory fee, provided members with a range of medical services. These
entities were typically linked to a specific industrial sector, such as railway
workers, police or teachers.
Today’s private health insurance sector comprises some 37 registered
private health insurers, a mix of not-for-profit insurers (mutual
organisations) and for-profit insurers. This number also includes restricted
membership funds which only provide cover to members of a specified
industry or group. Private health insurers must comply with regulatory and
prudential standards, including those listed below. Private health insurers can
operate nationally, or be based in a particular jurisdiction or region.
According to industry regulator APRA, in 2015–16
private health insurers paid nearly $19 billion in benefits to members (see tab
‘Fin Perf’). Of this $14 billion in benefits was paid for hospital treatment which
includes treatment in private hospitals, public hospitals, day hospitals and
hospital substitute treatment (see tab ‘Bens by Cat’). Revenue (primarily from
premiums, but also from investments) totalled around $22.5 billion. Management
expenses totalled around $1.9 billion, or 8.5 per cent of total revenue (see
tab ‘Fin Perf’).
Legislation and governance
Private health insurance is regulated primarily under the
Private
Health Insurance Act 2007 , the Private Health
Insurance (Prudential Supervision) Act 2015, and related rules and regulations.
Private health insurance is administered by the Department of Health with
prudential oversight provided by the Australian Prudential
Regulation Authority (APRA), a role previously performed by the Private
Health Insurance Administration Council. Consumer complaints are handled by the
Private
Health Insurance Ombudsman, which sits within the Office of the Commonwealth
Ombudsman and produces a State
of the Health Funds report annually. Broader consumer and competition
issues are dealt with by the Australian
Consumer and Competition Commission (ACCC), which also provides annual
reports on the sector to the Senate.
Types of private health insurance
There are two types of private health insurance: hospital,
and general treatment (sometimes called ancillary or extras)—or these can be
combined. Private health insurance does not cover services that are provided
out of hospital and which are covered by Medicare, such as general practitioner
services. Private health insurance coverage for the cost of ambulance
services varies across jurisdictions. Private health insurance is available
for singles,
couples, and families.
Private hospital cover
Private hospital insurance only covers services for which a
Medicare benefit is payable, as listed in the Medical Benefits Schedule
(MBS). Services not listed in the MBS, such as plastic surgery for cosmetic
reasons, are not covered by private health insurance. Hospital cover includes hospital
substitute treatment, such as hospital-in-the-home care (subject to medical
approval).
Medicare covers 75 per cent of the listed Medicare fee for hospital
services; private hospital insurance covers the remaining 25 per cent (known as
‘the gap’). Private hospital insurance may cover part or all of any amount charged
above the gap, and some or
all of the costs of accommodation and operating theatre fees, drugs,
prostheses, and diagnostic tests, depending on the policy and whether the
insurer has agreements
with hospitals.
Broadly, four levels
of private hospital cover are offered, with varying levels of exclusions
or restrictions:
- public cover—covers the lowest benefit permitted in a public
hospital, but the patient retains a choice of doctor
- basic cover—low level benefit covering a minimal number of
services with a range of exclusions and out-of-pocket costs
- medium cover—includes some restrictions and exclusions, but
covers a broader range than basic cover and offers lower benefits than top
cover and
- top cover—comprehensive; must cover all services listed in the
MBS.
The National
Health Reform Agreement allows patients with private hospital insurance who
are admitted to a public hospital to choose whether to be admitted as a public
or private patient. A recent report
from the Independent Hospital Pricing Authority shows that the proportion
of public hospital activity funded through private health insurance has grown
in recent years and suggests this is driven by public hospitals encouraging patients
to use their private cover. This has prompted the Australian
Private Hospitals Association to express concern that this may drive up the
cost of private health insurance premiums, while the Health
Minister Greg Hunt said he would be concerned if this lengthened public hospital
waiting lists.
General or ancillary cover
General treatment (or ancillary or extras cover) provides benefits
for out-of-hospital services such as dental, optical, physiotherapy, natural
therapies and non-Pharmaceutical Benefits Scheme medicines.
Membership levels
According to APRA
statistics, as at March 2017 some 11.4 million Australians had private
hospital cover (around 46.5 per cent of the population) and 13.5 million had
ancillary or general cover (around 55.5 per cent of the population).
Private health insurance membership as a proportion of
population initially fell after Medicare was introduced in 1984 (see chart below
from APRA). However, following the introduction of measures to encourage
membership, the proportion covered increased. Since September 2015, private
hospital coverage as a proportion of the population has declined from
47.4 per cent to 46.5 per cent.
Hospital treatment coverage
(insured persons as a proportion of population)
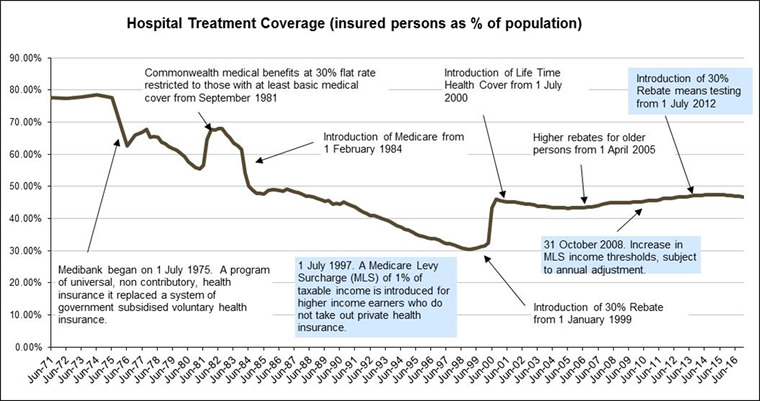
Source: APRA
Complexity of products
Private health insurance is becoming more complex. A range
of different co-payments, exclusions and restrictions can apply, making it
increasingly difficult for consumers to choose a suitable policy. The number of
insurance products on offer is not clear either. In the ACCC’s 2014–15
report to the Senate, it estimated there were around 46,500 private health
insurance products as at June 2015 (p. 35). More recently, the Private
Health Insurance Ombudsman clarified that this estimate (based on the
number of Standard
Information Statements (SIS) which
summarise the key product features) included products that are no longer
available. Removing these brings the total number of SISs to 27,281 as at January
2017, but this also includes products offered by restricted membership funds.
The government
advises consumers to shop around for the best value. Consumers can use a government website to
compare policies, or they can use a number of commercial comparator websites. However,
according to a recent
Choice survey, consumers still report difficulties in comparing
policies.
Consumer incentives and penalties
As already noted, a number of government incentives and
penalties apply to encourage greater participation in private health insurance.
These are explained briefly below.
Lifetime Health Cover
Introduced by the Howard Government in July 2000, Lifetime
Health Cover (LHC) is a two per cent annual loading on the cost of premiums
for people over 31 who delay taking out private health insurance. The maximum
loading is 70 per cent. It means that a person who takes out hospital cover at
age 40 for the first time will pay 20 per cent more on their premium than
someone who buys the same hospital cover at age 30. After ten years of
continuous cover any LHC will cease to apply. Those with LHC are allowed
specified ‘permitted days’ without cover. For example, if they travel overseas
they can choose to be without hospital cover for periods totalling 1,094 days
(or three years).
According to the latest industry
statistics, in March 2017 some 13 per cent of adult policyholders had
incurred a LHC loading.
Private health insurance rebate
The private
health insurance rebate is an income-tested government rebate on the cost
of private health insurance premiums for hospital, general treatment and
ambulance policies. Introduced in 1999, the rebate originally provided a 30 per
cent discount on premiums for those under 65, with higher rebates for older
Australians. Income testing was introduced in 2012, resulting in those on incomes
above an indexed threshold receiving a lower rebate or no rebate at all. From
2014, the calculation
of the rebate changed from a flat 30 per cent (higher for older
policyholders) to the difference between the Consumer Price Index (CPI) and the
industry weighted average increase in premiums. Over time, this has resulted in
a lower
rebate being available. Income
tiers and their applicable rebate levels are published by the Government each
year from 1 April. The income tiers used for income testing are normally
indexed annually, but were frozen at 2014–15 levels until 2018 as part of a Budget
Savings Measure. The Government announced in the 2016–17
Budget that it would maintain the freeze until 2021. Legislation
to enact this extension was passed in September 2016.
Medicare Levy Surcharge
The Medicare
Levy Surcharge (MLS) is an additional levy (on top of the 2.0 per cent
Medicare levy) imposed on high-income earners who decline to purchase private
health insurance. The surcharge is calculated at a rate of between 1.0 to 1.5
per cent of income.
The same budget savings measure which froze the income tiers
for the private health insurance rebate has also frozen the income tiers for
the purpose of determining liability for the MLS.
Features of private health
insurance in Australia
Private health insurance in Australia has some notable legislated
features.
Community rating
Private
health insurance in Australia is community rated, not risk rated like other
insurance products such as life insurance. Community rating requires that private
health insurance policies be offered at the same price irrespective of an individual’s
risk factors such as age (apart from the LHC age loading), health status,
previous claiming history or how frequently they need health care. Private
health insurers participate in a risk
equalisation scheme which partially compensates insurers with a riskier
membership profile.
Portability and waiting times
The portability
rule allows consumers to switch to another policy with a different insurer without
incurring additional waiting times, provided the new policy offers the same
level of benefits as their old policy. Certain limits and restrictions apply. Private
health insurers can impose a 12-month waiting period before hospital benefits can
be claimed by a newly joined member or someone upgrading to more expensive
cover if the person has signs or symptoms of a pre-existing
condition. A 12-month waiting period for obstetrics, and a two month
waiting period for psychiatric care, rehabilitation, palliative care and other
services on new or upgrading members can also be applied.
If a person has already served out part of a waiting period
on their previous policy, the remainder of the waiting period will apply on the
new policy, provided there are no added benefits or better conditions under the
new policy.
Broader Health Cover
Private health insurers can also offer coverage for hospital
substitute treatment (such as hospital-in-the-home)
and programs to help manage chronic diseases, under Broader
Health Cover arrangements.
Private health insurance reforms
The Private
Health Ministerial Advisory Committee was established in September 2016 to
advise the Minister for Health on a range of reform options. Its Terms
of Reference include developing simpler categories of insurance (such as
gold, silver, bronze), empowering consumer choice, transparency and
affordability improvements, improving value for rural and regional consumers,
alternative funding models for general treatment and other issues as directed
by the minister. The Committee was established following a consultation
process in 2015–16 and a consumer survey which revealed a number of
consumer concerns with private health insurance.
Separately, the Senate Community Affairs Legislation Committee is
undertaking an inquiry into the value
and affordability of private health insurance and out-of-pocket medical costs.
For copyright reasons some linked items are only available to members of Parliament.
© Commonwealth of Australia

Creative Commons
With the exception of the Commonwealth Coat of Arms, and to the extent that copyright subsists in a third party, this publication, its logo and front page design are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Australia licence.
In essence, you are free to copy and communicate this work in its current form for all non-commercial purposes, as long as you attribute the work to the author and abide by the other licence terms. The work cannot be adapted or modified in any way. Content from this publication should be attributed in the following way: Author(s), Title of publication, Series Name and No, Publisher, Date.
To the extent that copyright subsists in third party quotes it remains with the original owner and permission may be required to reuse the material.
Inquiries regarding the licence and any use of the publication are welcome to webmanager@aph.gov.au.
This work has been prepared to support the work of the Australian Parliament using information available at the time of production. The views expressed do not reflect an official position of the Parliamentary Library, nor do they constitute professional legal opinion.
Any concerns or complaints should be directed to the Parliamentary Librarian. Parliamentary Library staff are available to discuss the contents of publications with Senators and Members and their staff. To access this service, clients may contact the author or the Library‘s Central Enquiry Point for referral.