Use of MRI in Australia
Introduction
3.1
Magnetic Resonance Imaging (MRI) uses a powerful magnet and
radio-frequency pulses to collect signals which are processed by a computer to form
an image of part of the body.[1]
MRI is most effective for high level diagnosis of diseases of the
musculoskeletal system and central nervous system; early detection of tumours
and other abnormalities in areas such as the breast, prostate, spinal cord and
brain; and staging tests for various cancers.[2]
3.2
MRI is the only modality of diagnostic imaging in Australia which
operates under a licensing system. Two factors must exist in order for an MRI
scan to be eligible for Medicare Benefit Schedule (MBS) rebates:
-
the type of scan must be included on the MBS; and
-
the MRI machine must by fully or partially licensed.[3]
3.3
The unique licensing system of MRI in Australia was a prominent concern
of many submitters and witnesses throughout the committee's inquiry.
Stakeholders suggested that the licensing system was outdated, limited patient
access to MRI, resulted in significant costs for patients, and even delayed the
diagnosis and treatment of a patient's condition.
3.4
The Royal Australian and New Zealand College of Radiologists (RANZCR) informed
the committee that reform was needed in order to improve patient access to MRI
in Australia:
The current system of limiting Medicare rebates to particular
machines is restricting patient access and must be reformed. There is no
transparency from the Commonwealth government over criteria for new machines to
become eligible for rebates under the Medicare system. RANZCR believes that the
rules for MRI services in Australia must change to significantly increase
access, support and patient management and thereby improve clinical outcomes.[4]
3.5
This chapter will outline the number of MRI machines in Australia, the process
for referring a patient for an MRI scan, accessibility issues and the impact
this has on both patients and the health system. It will also highlight a number
of access and distribution issues relating to MRI machines, similar to those
discussed in chapter two.
Availability of MRI
MRI licensing system
3.6
MRI items were first listed on the MBS in 1998 with all 38 MRI machines
operating in Australia at the time granted eligibility for MBS items.[5]
The method of allocating eligibility has changed over time and included open
tender, invitation to apply and direct listings, however, there is currently no
open process to apply for an MRI licence.[6]
A graph outlining the expansion of MBS eligible MRI machines between 1998 and
2017 is at Appendix 4.
3.7
MRI licences are conferred by the Health Insurance (Diagnostic Imaging
Services Table) Regulations 2017 (DIST) through a Deed of Undertaking between
the MRI provider and the Commonwealth. The licence grants MBS eligibility to a
specific provider, in a specified location for a specific machine.[7]
3.8
Licences are granted on a full or partial basis. MRI machines with a
full licence attract a Medicare rebate on all MRI services listed on the MBS,
whereas MRI machines with a partial licence only attract a Medicare rebate on a
small subset of items listed on the MBS.[8]
3.9
As at 30 September 2017, there were 348 Medicare licensed MRI
machines in operation in Australia, 174 fully licensed and 174 partially
licensed.[9]
In addition, there are approximately 160 unlicensed MRI machines across
Australia which are privately funded and incur out-of-pocket expenses for
patients.[10]
3.10
The last major expansion of MRI licences occurred in 2012 when 46 full
and 179 partial licences were issued.[11]
Since 2013, only four additional licences have been issued. These licences were
granted at the discretion of government or on the basis of an election
commitment.[12]
There is currently no open application process to obtain an MRI licence. It is
not clear on what basis full and partial licences were previously allocated.
3.11
While MRI licences are granted by the Commonwealth, the Department of
Health (Department) noted that the Commonwealth Government does not determine
the location of diagnostic imaging equipment.[13]
Decisions regarding the location of public diagnostic imaging facilities are
made by state and territory governments and the location of private diagnostic
imaging facilities are commercial decisions.[14]
However, the Commonwealth Government requires that MRI machines be located in a
comprehensive radiology practice which also offers x-ray, ultrasound and computed
tomography (CT) services.[15]
3.12
The Department advised that there are 1.4 MRI machines eligible for
Medicare benefits per 100 000 population in Australia.[16]
The availability of licensed MRI machines in each state and territory is
summarised in Table 3.1 below.
Table
3.1: Medicare eligible MRI equipment by state and territory as at
30 September 2017
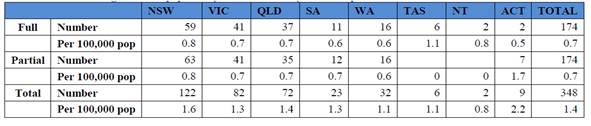
Source: Department
of Health, Submission 18, p. 16.
3.13
The Organisation for Economic Co-operation and Development (OECD) ranked
Australia 20th in the number of MRI machines per million population,
compared to 11th in the number of CT machines which do not face the
same accessibility and MBS restrictions.[17]
3.14
Furthermore, Australia's utilisation rate of MRI is disproportionately
low compared to the number of MRI machines. In 2015, Australia performed 41 MRI
scans per 1000 inhabitants, far less than comparable OECD nations such as
Canada, and France, and despite Australia having a greater number of MRI units
per million population.[18]
3.15
Professor Khangure from the Australian Medical Association (AMA)
attributed the higher utilisation of MRI in European nations to evolutions in
MRI technology which have improved the efficacy of MRI investigations and the
lack of radiation emitted by MRI, meaning it is safer for the patient.[19]
However, Professor Khangure explained that MRI may not be as widely used in
Australia, either because MRI machines are not available or because patients
must pay out-of-pocket if there is not an MBS subsidy for the required MRI
scan.[20]
As outlined further below, this often results in patients being exposed to a
radiation-related investigation, such as a CT scan, rather than an MRI which
does not emit radiation, and may increase the patient's risk of cancer.[21]
3.16
RANZCR expressed the view that while the locations of MRI machines have
not quite kept up with recent changes in population in some areas, they are
spread relatively evenly between each state.[22]
However, RANZCR also noted that focusing on the individual location of MRI
machines will not address the systemic issues associated with the accessibility
of MRI.[23]
3.17
The Department informed the committee that on 30 August 2017 the
Minister for Health requested that the Department undertake a review of the
distribution and availability of MRI licences.[24]
The Department advised that options on how the number of MRI licences may be
expanded have been provided to the Minister for Health for consideration.[25]
MRI referral pathways
3.18
At the heart of submitters and witnesses concerns was the way in which
patients are referred for an MRI scan under the MRI licensing system.
3.19
General practitioners (GPs) can only provide patients with a referral to
a partially licenced MRI machine for a sub-set of items listed on the MBS.[26]
These items include specified GP requested items, a range of cancer staging
services, Poly Implant Prosthese (PIP) breast items, Crohn's disease items and any
new items added to the MBS on the recommendations of the Medical Services
Advisory Committee (MSAC).[27]
However, this subset represents only 45 of the 193 MRI items listed on the MBS.[28]
3.20
By contrast, medical specialists are only able to refer patients to a
fully licensed MRI machine, but can refer the patient for the full range of MRI
items listed on the MBS.[29]
3.21
RANZCR explained that in an unrestricted market, referrers would funnel
their patients towards the best or newest MRI machine. However, under the
licence system, anomalies are created in which the opposite occurs, resulting
in patients being referred to an older MRI machine because it has a licence and
is eligible for a Medicare rebate.[30]
3.22 Envision Medical Imaging expressed concern that when coupled with the
capital sensitivity measure (discussed further in chapter five), the current
MRI licensing system left no financial incentive to upgrade MRI equipment prior
to the required 15 years.[31]
Envision Medical Imaging submitted that this resulted in Medicare eligible
scans being conducted on older MRI equipment, rather than the newest available
technology, and represented a poor return on investment for the Commonwealth's
funding of Medicare scans.[32]
3.23
Cancer Voices Australia submitted that the referral pathway between GPs
and specialists added an extra layer of complexity and it is very difficult for
patients to know where they can access a Medicare eligible MRI scan.
Accessibility of MRI
3.24
The committee heard that the MRI licensing system has a significant
impact on the accessibility and utilisation of MRI across Australia. The
committee notes that MRI accounted for only four per cent of diagnostic imaging
MBS services claimed in 2016-17.[33]
3.25
Submitters and witnesses maintained that the current MRI licensing
system, rather than the geographic location of machines, has the greatest impact
on the accessibility of MRI across Australia.[34]
Synergy Medical Imaging Pty Ltd submitted that 'the ability for patients and
referrers to choose their preferred imaging provider for MRI examinations is
compromised by the current system which restricts access to Medicare eligible
services.'[35]
3.26
Similarly, Professor Khangure expressed the view that the current MRI licensing
system only exists to ration services, rather than on the basis of clinical
need or evidenced-based care.[36]
Envision Medical Imaging agreed that the licensing system was initially
intended to limit the cost of MRI to the Medicare system by restricting the
referral and type of scans eligible for a Medicare rebate through the MBS.[37]
3.27
RANZCR directly attributed the issues surrounding the accessibility and
low utilisation of MRI to the licensing system. For example, Dr Slater noted
that the lack of restriction to CT scans often results in patients being
referred for a CT scan, even in circumstances when an MRI may be more appropriate,
as a Medicare eligible MRI scan may not be accessible to the patient or their
doctor.[38]
Dr Slater also noted that in instances where this occurs to young people and
children, they are particularly susceptible to subsequent cancers from exposure
to radiation through the CT scan.[39]
3.28
Professor John Magnussen from Macquarie Medical Imaging explained that
the current Commonwealth subsidy does not address the geographic disparity in
access to either equipment or expertise:
The current arrangements suffer from historical biases, as
you've already heard from previous submissions, potentially oversubscribing to
CT and geographically and diagnostically rationing the provision of MRI. This
leads to unavailability and inaccessibility of vital imaging services due to
the out-of-pocket expenses and travel to reach those services that are not
subsidised by the Commonwealth.[40]
3.29
By way of example, Envision Medical Imaging noted that the population of
Perth has increased by approximately 40 per cent, or 700 000 people since 2007,
yet no new full MRI licences have been issued in the past ten years.[41]
Envision Medical Imaging explained that the licensing system has created
inequities in the accessibility of MRI in Perth:
For instance, there are currently 12 privately owned
partially licensed MRI units in Perth compared with only 8 full licensed MRIs.
In effect, GPs and their patients have greater choice in determining where they
will have their scans and have shorter wait times and out of pocket gaps
associated with those scans compared with specialists and their patients who
are subject to less choice, longer wait times and higher out of pocket costs.[42]
3.30
Similarly, Perth Radiological Clinic submitted that the allocation of a partial
MRI licence to St John of God Midland Public and Private Hospital (Midland
Hospital) meant that only public inpatients could access an MRI at no cost
whereas private patients must pay out-of-pocket.[43]
Perth Radiological Clinic explained that a private inpatient's health insurer
is also not required to cover the cost of the MRI, meaning private inpatients who
contribute to their health care through the private health insurance system must
pay for an MRI at the Midland Hospital due to the licensing system.[44]
3.31
Furthermore, while a number of medical specialists have been attracted
to the area since the Midland Hospital opened in 2015, they are unable to refer
their patients to the hospital as it only holds a partial MRI licence, and not
a full licence, creating significant confusion for medical specialists and
restricting access for their patients.[45]
3.32
Mr Jim Aspinwall, Director of X-Ray and Imaging located on the Sunshine
Coast, Queensland suggested that historically MRI machines have been located in
affluent areas around Australia where patients are more likely to be able to
afford out-of-pocket costs.[46]
Mr Aspinwall explained that as MRI machines became widely used, private
radiology practices invested in their own machines independent of the licence
system:
If we're going to put in a machine and spend $1½ million to
$2 million on the machine and the only funding it's ever going to receive comes
out of patients' pockets, we're only going to put that into an area where we
think people might be able to afford to pay.[47]
3.33
Consequently, this has led to less affluent suburbs having poorer access
to MRI machines and resulted in longer wait times for these patients to receive
a Medicare eligible scan.[48]
3.34
Mr Mark Nevin of RANZCR acknowledged that while it is not practical for
an MRI machine to be available in every town across Australia, the current
distinction between fully and partially licenced machines restricts the
accessibility of MRI machines:
In general terms, with diagnostic imaging equipment, you
can't make an MRI machine available in every town in the country, so some
patients are always going to have to travel a little bit to access services.
But, at present, the fact that they have this distinction between being fully
eligible and being partially eligible means that it's confusing for patients as
to where they can get access to a service if they need an MRI, and it's also
confusing... for referrers as to where their patients can get access to an MRI
when they need that clinical information. [49]
Rural and regional accessibility
3.35
The Australian College of Rural and Remote Medicine (ACRRM) submitted
that poor access to diagnostic imaging services contributes significantly to
poorer health outcomes in rural and remote communities.[50]
In addition, patients in rural and remote areas frequently face higher out of
pocket costs as a result of undertaking travel for diagnostic imaging. This has
the potential to further delay their diagnosis and treatment and can have a
deleterious effect on health outcomes compared to patients in metropolitan
areas.[51]
3.36
Women's Healthcare Australasia and Children's Healthcare Australasia informed
the committee that MRI services in regional Western Australia, far western New
South Wales and the Northern Territory are particularly poor.[52]
Submitters also suggested that there were shortages or issues relating to access
to licensed MRI machines in a number of locations, including:
-
Queensland—northern Brisbane,[53]
Morayfield and Caboolture,[54]
Redcliffe and Sunshine Coast;[55]
Toowoomba;[56]
Wide Bay;[57]
Gladstone and Emerald[58]
and regional Queensland;[59]
-
New South Wales—northern beaches of Sydney;[60]
western Sydney,[61]
northern New South Wales,[62]
Cessnock;[63]
-
Victoria—western Melbourne;[64]
-
Western Australia—Kalgoorlie,[65]
Pilbara and areas north of Geraldton.[66]
3.37
The committee notes that this is not an exhaustive list of places with
access issues, but provides an indication of the areas identified by submitters
and witnesses.
3.38
Synergy Medical Imaging Pty Ltd, a private, independent radiology
practice in Cessnock, New South Wales, expressed concern that patients within
their electorate must travel approximately 43 kilometres to the nearest
Medicare eligible MRI machine. Alternatively, the nearest privately owned MRI
machine is 30 kilometres away where patients must pay out-of-pocket.[67]
3.39
Synergy Medical Imaging Pty Ltd noted that there has been no significant
improvement in the availability of MRI services since 2012, despite the fact
that there has been a shift in the demographics of the region, resulting in an
increase in demand for high quality healthcare services.[68]
3.40
Similarly, in the Sunshine Coast region north of Brisbane, the
electorate of Longman has a population of 159 345 people and only one full MRI
licence.[69]
As medical specialists are only able to refer patients to MRI machines with a
full licence, specialists have priority access to the only MRI machine in the
Longman, effectively precluding GPs from referring patients for an MRI within
their electorate.[70]
This is in stark contrast to the neighbouring electorate of Fisher which has seven
MRI licences, equating to a population of just 19 886 per MRI licence.[71]
3.41
The committee also heard that patients in regional Western Australia
have limited access to MRI:
Patients then have to travel to Perth if they are in the
northern part of Western Australia. Currently we have MRI equipment in
Geraldton but nothing further north. We have country MRI in Bunbury and Albany
but nothing in Kalgoorlie. If these patients need a clinical service or they
need something imaged, they actually have to travel to Perth to get that
information. If you could do it locally then at least you could decide whether
the treatment can be offered remotely or whether they need to be referred. At
this point in time they don't have an option; they have to travel to Perth.
They have CT in some of these locations. They have ultrasound and plain X-rays but
no access to MRI.[72]
3.42
WA Country Health Service told the committee that the travel burden for
regional patients is significant and should be taken into account when
considering any further expansion of Medicare eligible MRI machines.[73]
Committee view
3.43
The committee notes that there is no formal process available to apply
for an MRI licence and that consequently, the distribution of licenced MRI
machines does not account for recent population growth.
3.44
The committee is concerned that the MRI licensing system creates
confusion for patients and medical professionals alike and limits the accessibility
of MRI.
3.45
The committee agrees that the MRI licensing system has had a significant
impact on the accessibility of MRI for both metropolitan and rural and regional
patients and that this may have contributed to the underutilisation of MRI in
Australia.
3.46
The committee is concerned by reports that referral restrictions on MRI
scans has skewed GPs towards the use of CT, which is not restricted, and has
potentially compromised the clinically optimal diagnostic imaging and care of
patients.
Impact on patients
3.47
The committee heard that the current MRI licensing system leads to
patients travelling to receive a Medicare eligible MRI scan, increases out of
pocket costs, potentially delays diagnosis and has a particular impact on the
diagnosis of children.
Out-of-pocket costs
3.48
The committee heard that the restrictive MRI licensing system results in
out-of-pocket costs for patients for the MRI scan itself and for costs
associated with seeing a medical specialist in order to be referred for a
certain scan and potentially travelling long distances to access a Medicare
eligible MRI scan in a timely manner.[74]
3.49
New South Wales Health submitted that a gap payment may be charged by
private providers for an MBS eligible scan, even when the scan is performed by
an MBS eligible MRI machine as the Medicare rebate may not reflect the actual
cost of performing the scan.[75]
3.50
The Australian Diagnostic Imaging Association (ADIA) informed the
committee that between 2010-11 and 2015-16, the average gap payment between the
Medicare rebate and amount charged for an MRI scan has increased from $143 to $184.[76]
This is significantly more than the average out-of-pocket cost for diagnostic
imaging services in 2016-17 of $97.11.[77]
3.51
As discussed further in chapter five, there are a number of MRI scans
which are considered standard of care but are not included on the MBS and are
therefore not eligible for a Medicare rebate. Scans can only be added to the
MBS on the advice of MSAC, and at this stage these scans have not received MSAC
recommendation.
3.52
For example, Breast Cancer Network Australia (BCNA) submitted that as a breast
MRI is not included on the MBS, patients face high out-of-pocket costs for this
scan which varies significantly between radiology practices.[78]
In response to a survey conducted by BCNA, a respondent noted that 'my surgeon
recommends having an MRI but it is very expensive. It seems unfair that this
valuable test is only available to women who can afford it.'[79]
3.53
Research conducted by Deloitte Access Economics showed that a breast MRI
can cost between $450 and $1500 and over half of women paid at least $753 for
the MRI scan.[80]
BCNA added that young women who are diagnosed with breast cancer face further
financial strain as they often do not have the life savings which older women
have to fund their treatment.[81]
3.54
Similarly, the Prostate Cancer Foundation of Australia told the
committee that there is currently no Medicare rebate for a multiparametric MRI
which results in patients paying approximately $500–$600 per scan.[82]
Associate Professor Lowe noted that prostate cancer patients are often retirees
and therefore the out-of-pocket costs represent a substantial amount compared
to a working age person.[83]
3.55
An individual told Rare Cancers Australia that their grandfather had to
travel significant distance to receive an MRI scan with the associated travel
costs representing a further financial burden, in addition to the cost of the
MRI:
My grandfather had to travel 3 hours each way for his first
MRI scan, at which point neither his scan or petrol costs or anything were
covered, despite getting a cancer diagnosis from the MRI.[84]
3.56
Dr Evan Jones, Director of Morayfield Family Doctors in Queensland,
explained that the current licensing system can generate further out-of-pocket
costs for patients as GPs often refer patients to a specialist, at a cost to
the patient, as only the specialist can refer the patient for a scan on a fully
licenced MRI machine.[85]
Dr Jones explained that:
...GPs are restricted from ordering MRIs on a range of
conditions. Therefore, to get an MRI under a Medicare rebate they have to be
referred to a specialist. To see, say, an orthopaedic specialist privately they
might have to pay $400 or $450. That is a lot of out-of-pocket cost to see the
specialist, who will see them and say, 'You need an MRI' and fill out the MRI
form, and then they have to wait, have the MRI, wait for the next appointment
and pay the next bill to the orthopaedic surgeon or what have you.
3.57
The licensing system can also lead to out-of-pocket costs for patients
in a hospital with a partial MRI licence who require an MRI which only attracts
a Medicare rebate on a fully licenced MRI machine.[86]
UnitingCare Queensland explained that transporting patients to a fully licenced
MRI machine is often not possible and this results in a cost to the patient:
In times of emergency, particularly with brain or spinal
trauma where immediate access to an MRI scan is required, the last thing we
want to do is expose the patient to excessive and avoidable movement. It is
therefore in the patient's interest to conduct a full Medicare MRI scan, but
then the patient will be met with substantial out of pockets costs for doing
so. [...]
Even if patient transport is an option, the costs of doing so
are not minimal and utilise scarce resources that could no doubt be better
utilised elsewhere.[87]
3.58
The burden of out-of-pocket costs for an MRI scan can lead to patients
choosing to forego the scan or face extended waiting periods for a Medicare
eligible scan, if the scan required is listed on the MBS.[88]
Delayed diagnosis and treatment
3.59
Both out-of-pocket costs and the accessibility of an MRI can contribute
to a delay in the diagnosis and treatment of a patient's condition. Professor
Khangure explained that:
If they can't travel for whatever reason or the access is
through an unlicensed machine, that is another out-of-pocket cost, so it still
ends up a situation where the patient ends up with both a delay and a cost.
Sometimes they delay the investigation.[89]
3.60
Similarly, the committee was told that where patients cannot afford to
pay out-of-pocket for an MRI they may be forced to join long waiting lists
which prolongs the diagnosis and treatment of their illness:
They have to wait months just to get the outpatient clinic
appointment, then they would be waiting to get a diagnosis, then waiting to see
a specialist and then waiting for surgery.[90]
3.61
Cancer Council Northern Territory reported that patients can wait
between two and three weeks for an outpatient MRI scan which ultimately 'puts
significant delays in their cancer journey, the road to a definitive diagnosis,
delays to MDT [multidisciplinary team] discussion and treatment plan.'[91]
3.62
The committee heard that MRI is a 'one stop imaging shop' for the
diagnosis of many conditions but that restricted access to MRI can delay this
diagnosis.[92]
Dr Jones provided an example of a patient who went undiagnosed and
untreated for five years before undergoing an MRI scan:
He'd had lots of investigations. He'd had X-rays and he'd had
CT scans but he hadn't had the right investigation, which was an MRI. I
convinced him to spend the money and he went out and got an MRI and of course
what it showed was that he had widespread multiple sclerosis. That's a
37-year-old man who for five years has not been able to work. He now has
significant cognitive impairment: he has difficulties with memory; he has
difficulties with concentration. He will never be able to work again. If he'd
had the right diagnosis at the right time in the right way, we could have
instituted treatment and he could have continued with his life.[93]
3.63
Similarly, MS Research Australia (MSRA) submitted that the
diagnosis, ongoing monitoring and treatment of multiple sclerosis (MS) is
heavily reliant upon the use of MRI scans.[94]
MSRA explained that increased accessibility to MRI would reduce the delay in the
diagnosis of MS and hence improve outcomes for the initiation of treatment and
long term disability outcomes of patients with MS.[95]
3.64
As outlined in chapter two, repeated travel from rural and regional
locations to access an MRI scan and other diagnostic imaging services, further
delays the diagnosis and treatment of patients who do not live in metropolitan
areas.[96]
Impact on children
3.65
The committee also heard that the difficulties associated with accessing
MRI machines and the tendency instead towards performing CT scans has a
particular impact on children. Dr Slater explained that CT is not only an
inferior test to MRI, but that CT also exposes children to radiation:
The risk, firstly, is of the diagnosis not being made. A CT
is a test that is inferior to MRI for the diagnosis of brain pathology.
Secondly, there is the risk of radiation. Young people and children are
particularly susceptible to subsequent cancers from exposure to radiation in
their childhood. Thirdly, there's a risk that subsequent tests would still have
to be done to make the diagnosis. You heard the unfortunate situation where the
child might have a CT and would still end up having an MRI later.[97]
3.66
Similarly, Women's Healthcare Australasia (WHA) and Children's
Healthcare Australasia (CHA) submitted that the widespread use of CT as a proxy
to MRI, due to the lack of available MRI services, exposes children to high
levels of radiation.[98]
Associate Professor Susan Moloney, Member of CHA, informed the committee that
for approximately every 1000 CT scans performed on children, one child will
develop cancer.[99]
3.67
Dr Richard Zwar from the Peter MacCallum Cancer Centre noted that modern
CT scanners are dual energy which expose patients to significantly less
radiation, equivalent to only background radiation every individual receives.[100]
However, Associate Professor Moloney added that the varying ages and doses of
radiation from CT scanners still contribute to children developing cancer from
a CT scan, with machines in rural and regional Australia more likely to be older
and have higher radiation doses.[101]
3.68
Further restricting children's access to MRI is the time taken to
conduct the scan. An MRI scan requires children to stay still in a noisy
machine and can take between 45 minutes and an hour to complete, compared to
only 45 seconds for a CT scan.[102]
Therefore, children under the age of eight often require a general anaesthetic in
a tertiary medical centre to undergo an MRI scan, further limiting the accessibility
of MRI to children.[103]
3.69
Ms Julie Hale, Deputy Chief Executive Officer, CHA, noted that while
young children can undergo an MRI scan without general anaesthetic, this
requires time for the child to become acclimatised to the machine, and there is
no incentive to allocate additional time for a child's MRI scan under the
current system.[104]
Committee view
3.70
The committee recognises that the cost of an MRI scan can place a
significant financial burden on patients, often at a time when they are
severely injured or unwell, worsening an already stressful time in their lives.
3.71
The committee acknowledges that the out-of-pocket costs faced by
patients, in addition to the travel required to access a Medicare eligible MRI
scan, may delay or even prevent a patient receiving their diagnosis. The committee
notes that this can have devastating impacts for the patient and may have a
deleterious impact on the health system if the patient's condition worsens and
requires acute care in the future.
3.72
The committee is particularly concerned by reports that children are
being subjected to the radiation of CT scans due to issues associated with the
accessibility of MRI machines and a lack of incentive to accommodate the
additional time required for children.
Impact on the health system
3.73
The MRI licensing system and its impact on patients has ramifications
across the whole health system. Submitters and witnesses called for reform of
the MRI licence system, but recognised that any reform also requires
consideration of the effect on the broader health system.
Reforming the MRI licence process
3.74
A criticism put to the committee by submitters and witnesses was the
lack of an objective and transparent application process for new MRI licences.
Stakeholders were overwhelmingly in favour of reforming the current MRI licence
system and stressed the need for an objective and transparent process, but
differed somewhat on the proposed criteria for new licences. [105]
3.75
RANZCR submitted that GPs should have the ability to refer patients for
the full range of MRI scans to enable GPs to maintain management of their
patients and potentially avoid unnecessary specialist referrals, saving both
the patient and health system time and money.[106]
3.76
The AMA supported the idea that patients should be able to access an MRI
on the basis of clinical need, rather than through a licence system.[107]
3.77
Mr Dean Lewsham, Chief Executive, Primary Health Care Limited also
agreed that clinical need should be an aspect of an objective application
process but that consideration should also be given to the gap between accessibility
of MRI in regional and metropolitan areas.[108]
3.78
In order to address the accessibility of MRI in Australia, the Perth
Radiological Clinic suggested the introduction of an application process for
licences which responded to specific criteria including need in the community,
health demographics, level of disadvantage in the community, level of
investment for the equipment and a profile of the operating clinician.[109]
3.79
Similarly, New South Wales Health recommended that an area of need
approach, similar to the Commonwealth Government's radiation oncology health
program grant scheme, should be implemented to ensure that that the process
under which licences were granted promoted equity in access for all patients.[110]
3.80
A number of witnesses and submitters also questioned whether the
differentiation between partial and full licences should be removed. Cancer
Voices Australia recommended that all MRI machines be eligible for Medicare
rebates to ensure that all cancer patients in Australia have equal access to
MRI and are provided quality care.[111]
3.81
However, some witnesses were hesitant to suggest that the MRI licensing
system should be completely de-regulated as it would be very costly and may not
improve the outcome or accessibility for patients.[112]
3.82
Professor John Magnussen emphasised that any change to the MRI licensing
system should consider patient care as paramount:
And in all of this an important thing to remember is that we
have to aim for quality outcomes. We want to improve patient care, because if
we're not improving patient care, if we just open up licences everywhere, we
haven't achieved much but we've spent a lot of money.[113]
3.83
While MRI scans amounted to only four percent of MBS services claimed in
2016-17, this equated to a disproportionately high 13 per cent of all MBS benefits
paid.[114]
Therefore reform to the MRI licensing system is likely to have significant cost
implications.
3.84
The Department advised that upgrading all current partially licensed MRI
machines to a full licence would cost approximately $150 million per year.[115]
Full deregulation of the MRI licence system, including upgrading all partial
machines to a full licence and conferring eligibility on existing privately
operated MRI machines, would cost over $400 million per year if all machines
were operating at full capacity.[116]
Offsetting the cost to the health
system
3.85
The committee heard that the current MRI licensing system places
significant cost not only on patients, but also on the public health system.
This is a result of patients deferring medical care, receiving multiple tests
in place of MRI and the cost of transporting patients between hospitals for an
MRI scan on a licensed machine.
3.86
The AMA submitted that when people defer or avoid medical care due to
cost, there are consequences downstream in the health system.[117]
Professor Khangure explained that when diagnostic imaging is used appropriately
and effectively, it saves the health system money:
It saves money because it is critical to an early diagnosis,
treatment and disease monitoring. Early diagnosis and treatment and appropriate
monitoring prevent much higher downstream costs arising from more expensive
hospital stays and higher cost medical care.[118]
3.87
In regard to offsetting the cost of a potential increase in the use of
MRI, Professor Khangure explained that often the alternative diagnostic imaging
modality to an MRI is more than one test, such as a combined ultrasound and CT,
or an invasive hospital procedure, and that the cost to the health system must
be considered holistically:
The question is: what is the overall cost of health care, not
just the cost of the imaging component? If you reduce the overall cost in
health care by not having the patient hospitalised for a more invasive
procedure but the alternative is a little more expensive in investigation, the
overall cost structure is still less. It's a bit more complex than simply
saying that doing an MRI reduces the cost of imaging—it may not—but it reduces
the cost in health care, which is really the bit we need to be looking at.[119]
3.88
Mr Jim Aspinwall provided an example to the committee of a hypothetical
patient named Alan who presents at a local health hub with neurological
symptoms.[120]
Figure
3.1—Treatment pathways for patients with access to fully licensed MRI

Source: Mr Jim Aspinwall,
Director, X-ray and Imaging, MRI Licence Requirement Morayfield Health Hub,
p. 1 (tabled 13 December 2017).
Committee view
3.89
The committee is of the view that there is a need for reform of the MRI
licensing system. The committee is pleased that advice has been provided to the
Minister for Health regarding the distribution and availability of MRI
licences, including possible options for reform and urges the Minister to
urgently consider this information with a view to reform.
3.90
The committee recognises that an expansion in the number of MRI licences
may incur significant cost to the Australian government, but notes that these
costs may be offset elsewhere within the public health system.
Navigation: Previous Page | Contents | Next Page